STI Surges Over the Holidays What That Festive Season Warning Really Means for You
Quick Answer: Probiotics don’t prevent chlamydia. They support gut and vaginal health, but they can’t block the transmission of sexually transmitted infections. Testing and protection are still essential.
This Article Is for You If You’re Thinking “But I Take Care of Myself…”
If you’re someone who drinks your greens, tracks your cycle, eats fermented foods, and still got blindsided by an STD, this article is for you. Maybe you feel embarrassed. Maybe you’re confused, wasn’t this what wellness was supposed to prevent?
This is also for people in monogamous relationships who tested positive and are scared what it means, for anyone exploring sex again after a dry spell, and for every health-conscious person who thought immunity meant invincibility.
We’ll walk through why chlamydia happens even to the “healthy” ones, how probiotics help (but don’t protect), what tests are available, and how to take action that’s stigma-free and effective.

People are also reading: I Thought I Had Herpes, Turns Out I Was Wrong
Let’s Start With the Biology: What Chlamydia Actually Is
Chlamydia trachomatis is a bacterial infection, passed primarily through vaginal, anal, and oral sex. It’s one of the most common STDs globally, and it often causes no symptoms. According to the CDC, nearly 70% of women and 50% of men with chlamydia won’t notice anything wrong.
The bacteria infect the mucous membranes in your reproductive tract, urethra, rectum, or throat depending on how it was transmitted. Unlike your gut flora, this is not the kind of bacteria you want hanging around, it can lead to infertility, pelvic inflammatory disease, and testicular inflammation if left untreated.
So no, it’s not about how “healthy” your lifestyle is. It’s about whether bacteria entered your body during intimate contact, and whether you caught it in time with testing.
Probiotics 101: What They Actually Do (And Don’t)
Probiotics are living microorganisms, usually strains of Lactobacillus and Bifidobacterium, that help maintain the balance of “good” bacteria in your gut and, for those with vaginas, in your vaginal microbiome. They support digestion, immune modulation, and vaginal pH. That’s all real. What’s not real? The belief that they can prevent or treat bacterial STDs like chlamydia.
According to a 2019 study in the Journal of Clinical Medicine, probiotics can reduce recurrence rates of some vaginal infections, like bacterial vaginosis and yeast, but there is no evidence that they prevent or cure STDs. They simply don’t work that way. They modulate internal flora; they don’t shield mucous membranes from outside pathogens during sex.
Think of probiotics like housekeepers: they help clean up after the fact. But if someone breaks in during the night (i.e., bacterial transmission during sex), that’s a job for locks (condoms), cameras (awareness), and follow-up (testing).
What Probiotics Support vs What They Don’t
Table 1: Probiotics help with balance, not protection. They’re useful tools, but not substitutes for prevention methods when it comes to STDs like chlamydia.
“But I’ve Been Monogamous,”Other Ways Chlamydia Shows Up
This is where shame creeps in for a lot of readers. You’ve been exclusive. You haven’t “done anything risky.” So how the hell did this happen?
Here’s the truth: You can carry chlamydia silently for weeks or months. It may have been from a past relationship. Your partner may have had it and not known. Condoms don’t always fully protect against infections during oral sex or with incorrect use. And yes, occasionally, false negatives can happen in early tests or rapid testing without follow-up.
Chlamydia is sneaky. It’s not a reflection of your morals, cleanliness, or intelligence. It's a reflection of how easily this bacteria spreads, and how few people get tested until symptoms (or surprises) show up.
If you’re feeling betrayed, scared, or confused, all of that is valid. What matters most now is clarity, treatment, and taking the shame out of the equation.
Gut Health ≠ STI Immunity: Clearing Up the Confusion
There’s a seductive logic to the idea that if your immune system is strong, you won’t get sick, including with STDs. But sexually transmitted infections don’t work like colds. They aren’t “fought off” before infection takes hold. Chlamydia enters the cells lining your genitals, rectum, or throat. Once it’s in, no amount of probiotics can prevent colonization. Your body doesn’t recognize it as a threat fast enough, especially if you don’t show symptoms.
One 2020 study in Frontiers in Cellular and Infection Microbiology noted that while the immune system may eventually fight chlamydia, it’s often after damage has begun. Worse, immunity isn’t long-lasting, meaning you can get reinfected even after successful treatment. This makes testing, not “clean living”, your strongest line of defense.
So let’s reframe things: good immunity supports recovery, but only testing and protection prevent infection in the first place.
“I Do Yoga, I Eat Clean, I Still Got Chlamydia”
Jonah, 32, is a plant-based runner who hasn’t eaten processed food in years. “I don’t even drink,” he said. “My girlfriend and I were both taking probiotics. We thought we were doing everything right.”
When she tested positive during her routine pelvic exam, Jonah was stunned. “We hadn’t slept with anyone else in months. We’re super monogamous. It didn’t make sense.” His first instinct was to question the test. Then came the guilt.
“Was it me? Was it from before? Did we get false results? Did I give her something? It messed with my head.”
Jonah got tested, and sure enough, he was positive too. They had both been asymptomatic. Likely, one had it from a prior relationship, and it went undetected. Jonah now swears by at-home tests every six months, “even if nothing feels wrong.”
This isn’t rare. Most people who test positive for chlamydia feel blindsided. But it’s not about poor hygiene, or lack of morals, or ignoring health. It’s about how easily this infection flies under the radar.
How STDs Like Chlamydia Can Spread (Even If You're "Careful")
Table 2: Even careful, health-conscious people can be exposed to STDs like chlamydia. Prevention isn’t just about behavior, it’s about knowledge, testing, and timing.
Are There Any Probiotic Strains That Help With Chlamydia?
A lot of people ask this question on holistic health forums, and the short answer is no, not directly. Some new studies have looked into whether some strains of Lactobacillus can make the vagina a safer place, especially after treating infections like bacterial vaginosis (BV). But those benefits have more to do with getting your flora back to normal after taking antibiotics than with stopping the spread of chlamydia during sex.
Researchers are looking into using vaginal suppositories with probiotics as extra care, but these are not barriers, only extras. So far, no randomized controlled trial has shown that a probiotic, pill, yogurt, or capsule can stop chlamydia.
That doesn't mean they don't work; it just means they don't protect you. Use them to help you heal, not to replace condoms, conversations, or screenings.

People are also looking for: How to Use a Chlamydia Rapid Test at Home and Read the Results
Let’s Talk Retesting: What If You’ve Already Been Treated?
If you’ve had chlamydia before, you may wonder: how soon should I test again? Or is it possible I still have it? Here’s what most sexual health guidelines say:
- After treatment (usually a single dose or 7-day course of antibiotics), you should retest at 3 months, even if your partner was treated too.
- If you still have symptoms after treatment, or they return after new contact, retesting after 30–45 days is reasonable.
- Always retest if you’re starting a new relationship or if there’s any uncertainty about prior partners' status.
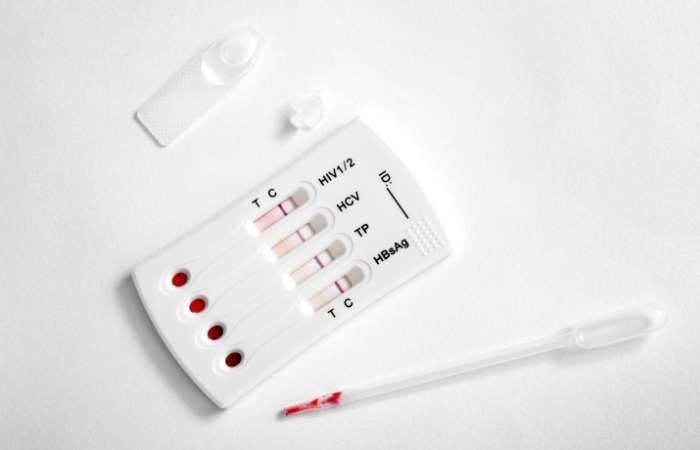
At-home testing is a low-stress way to do this. This combo test kit checks for the most common STDs and can give you peace of mind discreetly.
Why “Healthy” People Still Get STDs
There’s a cultural myth that STDs only happen to people who are reckless, dirty, or careless. That myth is not only wrong, it’s dangerous. It prevents people from getting tested, from talking openly with partners, and from seeking treatment without shame.
We’ve seen this with chlamydia over and over. People with gym memberships, clean diets, strong immune systems, and regular probiotic use still test positive. Why? Because STDs don’t care how clean your eating is. They care about exposure.
Your gut bacteria may be balanced. Your immune system may be strong. But no amount of internal health can override what happens during unprotected sex, oral contact, or exposure through toys or fluids. Being healthy doesn’t make you immune. It just makes you better equipped to handle life, including chlamydia treatment.
Does This Mean You Should Stop Taking Probiotics?
Absolutely not. Probiotics have many proven benefits for digestion, immunity, and vaginal flora. Some studies even suggest they may help reduce recurrence of infections after antibiotic treatment.
But taking them with the belief that they will “protect” you from sexually transmitted infections is like wearing sunscreen and thinking you can’t get a mosquito bite. Wrong tool. Right mindset. Just the wrong match.
Keep your probiotics. Just don’t let them give you a false sense of security when it comes to STD protection. For that, you need testing, barriers, and honest conversations.
What Actually Prevents Chlamydia?
If probiotics aren’t the answer, what is? Here’s what works, according to every major public health authority:
- Correct and consistent condom use during vaginal, anal, and oral sex
- Getting tested regularly, even when asymptomatic
- Mutual testing with new partners before becoming exclusive
- Using dental dams or barriers for oral sex or toy play
- Cleaning sex toys between uses and between partners
None of these are foolproof, but they significantly reduce your risk. And when you pair them with awareness and at-home STD testing, you’re giving yourself the best shot at staying safe without sacrificing intimacy.
What to Do If You Just Tested Positive
If you’re here because you just saw two lines on a rapid test, or got a call from your clinic, take a breath. You’re not alone. Millions of people test positive for chlamydia every year, and most recover completely with a short course of antibiotics.
Here’s what comes next:
- Take the full antibiotic course, even if you feel fine
- Don’t have sex until your treatment window is complete (usually 7 days after the last pill or injection)
- Let any recent partners know, either directly or via anonymous notification services
- Retest in 3 months to confirm you're clear
There’s no shame in getting an STD. The only shame would be letting stigma stop you from healing. And healing starts with knowledge.
People are also reading: STD Testing Regret: 10 Things I Wish I Knew the First Time
FAQs
1. Are probiotics able to stop chlamydia?
No, probiotics help the health of the gut and vagina, but they don't protect against chlamydia or other sexually transmitted infections. They don't make a barrier or immune response that keeps bacteria from getting into the body during sex.
2. Why did I get chlamydia if I take care of myself and am healthy?
Chlamydia is not spread by being sick; it is spread by having sex. People who are very clean, have strong immune systems, and live healthy lives can still get STDs. It's not your wellness routine that matters; it's your exposure.
3. Can gut health affect the prevention of STDs?
Not directly. Gut health can affect the immune system as a whole, but STDs like chlamydia can get around general immunity by infecting mucosal tissues. There is no proof that gut flora stops STDs from spreading.
4. Can probiotics help with or cure chlamydia?
No. Chlamydia needs antibiotics to treat it, usually azithromycin or doxycycline. Probiotics may help the gut heal after antibiotics, but they are not a replacement for medical treatment.
5. Does having chlamydia mean you have a weak immune system?
Not always. Chlamydia can infect anyone, no matter how strong their immune system is. You didn't get sick because your immune system failed; it spread because it was exposed and often went unnoticed.
6. While I'm treating chlamydia, can I take probiotics?
Yes. A lot of people take probiotics while they are on antibiotics to keep their gut in balance and lessen the side effects of antibiotics on their digestion. To avoid problems, just space out the doses by a few hours.
7. I took probiotics and tested negative at first, but then positive later. Why?
You might have tested during the window period, which is the time before the infection can be found. Or you were exposed again. Probiotics don't change how accurate STD tests are in either direction.
8. Is it possible for chlamydia to come back after treatment?
Yes. If your partner wasn't treated or if you come into contact with the virus again, you could get it again. That's why it's a good idea to test again in three months after a positive result.
9. Do certain strains of probiotics help keep the vagina healthy?
Some strains, such as Lactobacillus crispatus, may help keep the balance of vaginal flora and lower the risk of BV or yeast infections. But they don't stop STDs like chlamydia.
10. Should I still use at-home STD tests even if I don't have any symptoms?
Yes. Most people who have chlamydia don't have any symptoms. Regular screenings are important for finding and treating problems early, especially with new partners or after having sex without protection.
You’re Not “Too Clean” to Catch Chlamydia, You’re Just Human
It’s time to separate wellness culture from reality. You can eat the cleanest diet, take daily probiotics, and still test positive for chlamydia. That’s not failure. That’s biology. And knowing the difference can change everything.
Don’t let false security stop you from testing. And don’t let shame keep you from getting treated. This at-home combo test kit gives you clear answers fast, no clinic trip required. Wellness is honesty. Start with yourself.
How We Sourced This Article: We combined current guidance from leading medical organizations with peer-reviewed research and lived-experience reporting to make this guide practical, compassionate, and accurate. In total, around fifteen references informed the writing; below, we’ve highlighted five of the most relevant and reader-friendly sources.
Sources
1. Planned Parenthood – Chlamydia Overview
2. Lactobacillus Modulates Chlamydia Infectivity and Genital Tract Pathology in vitro and in vivo
3. Lactobacillus crispatus Inhibits the Infectivity of Chlamydia trachomatis Elementary Bodies
5. The Role of Probiotics in Women’s Health
About the Author
Dr. F. David, MD is a board-certified infectious disease specialist focused on STI prevention, diagnosis, and treatment. He blends clinical precision with a no-nonsense, sex-positive approach and is committed to expanding access for readers in both urban and off-grid settings.
Reviewed by: M. Patel, MPH | Last medically reviewed: September 2025
This article is for informational purposes and does not replace medical advice.







