Think It’s Just Irritation? These Chlamydia Symptoms Say Otherwise
Quick Answer: Some STDs can cause symptoms within a few days of exposure, including gonorrhea, herpes, and trichomoniasis. But even if you feel fine, early testing and retesting are key to catching infections that don’t wait, or don’t warn you at all.
This Guide Is for You If Last Night’s Still Haunting You
Maybe the condom broke. Maybe you didn’t use one at all. Maybe it was oral only and you thought that meant safer. Now you're dealing with burning, discharge, a weird bump, or worse, nothing at all except panic. This guide is for anyone who’s ever Googled “can you get an STD from one time?” while sitting on the toilet.
We’re not here to shame or scare you. This article is about information, not judgment. We’ll unpack the seven most likely culprits behind your sudden symptoms, or creeping anxiety, and explain what tests you need, when to take them, and what symptoms to watch for (or ignore). Because you deserve clarity, not chaos.
Whether you’re in a hookup culture, a long-term situationship, or just made one choice that’s now making you spiral, testing is care. Let’s get into what’s really going on under the surface.

People are also reading: You Got Tested… But Did They Actually Check for Everything?
How Fast Can an STD Show Up? Sooner Than You Think
There’s no one-size-fits-all timeline for STDs. Some show signs in 2–5 days. Others can take weeks, or stay completely silent. But just because symptoms are delayed doesn’t mean the infection isn’t active. In fact, many STDs are most contagious before they even cause noticeable symptoms.
Here’s a quick look at how fast seven common STDs can begin to cause symptoms after exposure, and when you should start thinking about testing.
Figure 1. Estimated onset and testing windows. Individual timelines may vary, especially if you're immunocompromised, pregnant, or have had prior infections.
Remember: the presence or absence of symptoms is not a reliable indicator of infection. Many people carry and transmit STDs without ever feeling a thing.
"We Only Hooked Up Once, But It Was Enough"
Renee, 25, met her date through an app. “It was one of those nights. We kissed, we laughed, we had sex, fast, unplanned, and unprotected. I didn’t think much of it until three days later when I started feeling this intense burning while peeing. At first, I thought UTI. But something told me to check for more.”
“Turns out it was gonorrhea. I was floored. I always assumed STDs took weeks to show up, or that you needed multiple partners to be at risk. Nope.”
Renee’s story isn’t rare. It’s not about “promiscuity.” It’s about biology, timing, and a virus or bacterium being in the right place at the wrong time. You don’t need a history. You don’t need symptoms. You just need one exposure.
If this feels close to home, you’re not being paranoid. You’re being proactive.
Herpes: When That Tingle Isn’t Just Anxiety
If you’ve got a tingling, itchy feeling near your genitals, or tiny bumps that look like blisters, it could be herpes. It often shows up fast, within 2–12 days of exposure. Some people also experience fever, fatigue, or swollen glands before the blisters appear.
The first outbreak is usually the most intense. After that, the virus can go dormant and resurface during times of stress or illness.
But here’s the kicker: you don’t need visible sores to have or transmit herpes. Many people carry HSV-2 or HSV-1 (yes, the kind that causes cold sores) without knowing it. Oral sex is a major transmission route for both.
Feeling off? You can test during an outbreak using a swab or take a blood test (IgG) after the 14-day mark. Earlier testing can give false negatives, so timing matters. If you're already seeing symptoms, now’s the time to act.
Gonorrhea: The Infection That Burns Fast and Spreads Faster
A burning sensation while peeing? Yellowish discharge you can’t ignore? Sore throat after oral sex? That could be gonorrhea. Symptoms often appear in just 2 to 5 days, and it’s one of the most easily transmitted STDs. Even if you used a condom for penetration, gonorrhea can still spread through oral sex, finger play, or shared toys.
Men often notice painful urination and discharge early. Women, however, might confuse symptoms with a UTI or miss them entirely, until it spreads to the pelvic area and causes more serious issues. Untreated, it can lead to infertility in all genders.
Gonorrhea is detected through a NAAT test, typically from urine or a vaginal/cervical swab. You can test as early as 7 days post-exposure, but 10–14 days is ideal for accurate results.
Chlamydia: The Silent Climber
Chlamydia is sneaky. It’s the most reported bacterial STD in the U.S. and often causes zero symptoms. But when it does? Think light spotting, testicular pain, or discomfort during sex or urination, often confused with other things. It typically surfaces around 7–21 days post-exposure.
Like gonorrhea, chlamydia can be caught from oral, anal, or vaginal sex, and yes, toys too. The test is simple: a urine sample or swab. You can test around day 10, but 14 days gives the most reliable result. Left untreated, it can damage reproductive organs and increase HIV risk.
Chlamydia also has a high reinfection rate. If a partner goes untreated, it can boomerang back to you, even after antibiotics.
Syphilis: The Painless Sore That Doesn’t Stay Quiet
Syphilis often starts with a single, painless sore on the genitals, mouth, or anus. This sore can show up 10 to 90 days after exposure and is easy to miss, especially if it’s internal or mistaken for a pimple or ingrown hair. But make no mistake: syphilis moves fast once it’s in your system.
Stage two can bring a full-body rash, flu-like symptoms, or swollen lymph nodes. Without treatment, it can damage your brain, nerves, and organs years later. It’s serious, but very treatable when caught early.
Testing involves a blood draw and is most accurate after 3–6 weeks. If you suspect exposure, especially to someone with symptoms or a known diagnosis, don’t wait. You can also test earlier and retest later if needed.
People are also reading: Yes, You Can Get Herpes Without Sex,Here’s How It Happens
Trichomoniasis: The Forgotten Infection That’s More Common Than You Think
Most people haven’t heard of trichomoniasis (aka “trich”), but it’s the most common non-viral STD. Caused by a parasite, trich can start causing symptoms within 5 to 28 days, though about 70% of people never notice anything.
When symptoms do appear, they often include frothy discharge, itching, irritation, and a strong odor. Men may notice irritation inside the penis, slight discharge, or burning after urination or ejaculation. Many dismiss it as nothing, and that’s where trouble starts.
Trich is easily diagnosed with a swab or urine test and treatable with a single dose of antibiotics. The problem? Most people never test because they don’t know it exists.
HIV: The Flu That Isn’t the Flu
Contrary to stigma, HIV doesn’t instantly “ruin your life.” But it does deserve respect, and early testing. Symptoms can appear within 2 to 4 weeks after exposure and often look like the flu: fever, chills, fatigue, sore throat, and body aches. That’s when your body is fighting acute HIV infection.
Early diagnosis means access to antiretroviral therapy (ART), which can reduce viral load to undetectable levels, making the virus untransmittable to partners. The sooner you know, the better the outcome for your health and relationships.
Testing options include Ag/Ab combo tests (detectable around 18–45 days) and NAAT tests (detectable around 10–33 days). At-home options exist but confirm with lab testing if you’re early in the window period.
HPV: The One You Can’t Really Test For (Unless You Have a Cervix)
HPV is incredibly common, and usually harmless. But some strains cause genital warts, while others lead to cancers of the cervix, throat, anus, and penis. It often takes 1–3 months for warts to appear after exposure, if at all. Most people clear HPV naturally, but persistent infections can cause long-term problems.
There’s no FDA-approved HPV test for people with penises. For those with a cervix, HPV screening usually starts around age 25 as part of a Pap/HPV co-test. If you notice new warts, irritation, or have a partner with known HPV, see a provider, even if you’re symptom-free.
The HPV vaccine is highly effective, but it doesn’t cover all strains. Condoms help reduce transmission, but HPV can spread through skin-to-skin contact, even with no penetration.
When Should You Test? It’s About Timing, Not Just Symptoms
Even if your symptoms show up fast, the tests don’t always catch the infection right away. That’s the window period, the time between exposure and when a test can accurately detect an infection. Test too soon and you might get a false negative, only to test positive days later.
Here’s the truth: if you’ve just had a risky encounter and you're feeling off, it’s valid to want answers now. But testing strategies should match each STD's window period. Let’s break it down in real-world terms.
Figure 2. Testing windows by exposure timing. These aren’t hard cutoffs, retesting and clinical judgment are always advised if symptoms persist.
If you’re within 14 days of exposure, test what you can, but know that a second test later can give you full clarity. Testing isn't one-and-done if the exposure was recent.
The Retesting Rule: Why One Negative Isn’t Always Enough
Let’s say you test on day six and everything comes back negative. That’s a relief, but it’s not a guarantee. Many people assume they’re in the clear and stop there. That’s a mistake, especially for infections like syphilis and HIV, which can evade detection during the early window.
Case scenario: Jordan took a combo STD test five days after a risky hookup. Everything was negative. Then, at day 20, a weird rash appeared on his palms. He got retested, and it came back positive for early syphilis. The timing mattered.
That’s why follow-up testing matters. Retest 2–4 weeks after the first round if you tested early, symptoms change, or your partner tests positive. You’re not being overly cautious, you’re being thorough. And that can make all the difference.
What If You Still Have Symptoms but Tested Negative?
This is one of the most common pain points. You did the “right” thing, took the test, but something still feels off. Maybe you’ve got a rash, discharge, or ongoing burning. So what now?
First: not all tests are created equal. A herpes blood test might miss a new infection. A urine-only test could miss oral or rectal infections. And window periods matter, too soon means it won’t show yet. In other words, your negative might be more about timing than truth.
Second: some symptoms aren’t caused by STDs at all. Yeast infections, bacterial vaginosis, allergic reactions, or non-STD urethritis can all mimic infection signs. If your symptoms persist, worsen, or change, follow up with a provider or retest using a different sample type (e.g., throat or rectal swab).
Bottom line: trust your body. If something feels wrong, you deserve answers, and that may mean a second look.
People are also reading: Is It Genital or Oral Herpes? Here’s How to Tell the Difference
When to Call in a Provider or Use Telehealth
Not every situation requires a clinic visit, but here’s when you should escalate:
- Symptoms are severe or spreading (e.g., fever, swollen lymph nodes, painful sores)
- You’re pregnant or trying to conceive
- You have a weakened immune system (HIV positive, on immunosuppressants, etc.)
- Your test is positive and you need prescription treatment
- Your partner just tested positive and you need guidance
Many at-home services now offer telehealth consults or prescription access after a positive result. The CDC’s STD resource page includes links to find local clinics and treatment pathways.
If you're not sure whether your test is enough, or if your symptoms match a non-STD issue, medical guidance can make all the difference.
FAQs
1. Can an STD really show up the next morning?
It’s rare, but yeah, some infections don’t wait around. Gonorrhea and herpes can sometimes cause symptoms within 48 hours, especially if your immune system is already stressed. But don’t bank on symptoms to tell the full story. Most STDs are sneakier than that.
2. We used a condom. Should I still be worried?
Honestly? It depends. Condoms do a great job at reducing risk, but not eliminating it. Skin-to-skin spreaders like herpes, HPV, and syphilis can slip through the cracks, literally. And if there was oral, fingers, or shared toys involved? Still possible. Protection is smart, not perfect.
3. I only gave (or got) oral. Can I still get something?
Big yes. Oral sex can transmit herpes, gonorrhea, syphilis, HPV, and even HIV in very rare cases. A sore throat after a spicy hookup? Might not be from the hot sauce. If your mouth or theirs was unprotected, testing still makes sense.
4. My test came back negative, but I still feel off. Now what?
Two words: window period. If you tested too soon, especially within the first 5 to 10 days, you could get a false negative. Or maybe your test didn’t include all sites (mouth, rectum). Some tests miss things. Trust your gut. Retest, or talk to a provider about symptoms that linger.
5. Is it possible to have an STD and feel totally fine?
Oh, absolutely. Chlamydia is a quiet one. So is trich. And HPV? Most people never feel a thing. You can walk around symptom-free and still pass it to someone else. That’s why regular testing matters, even if nothing feels “off.”
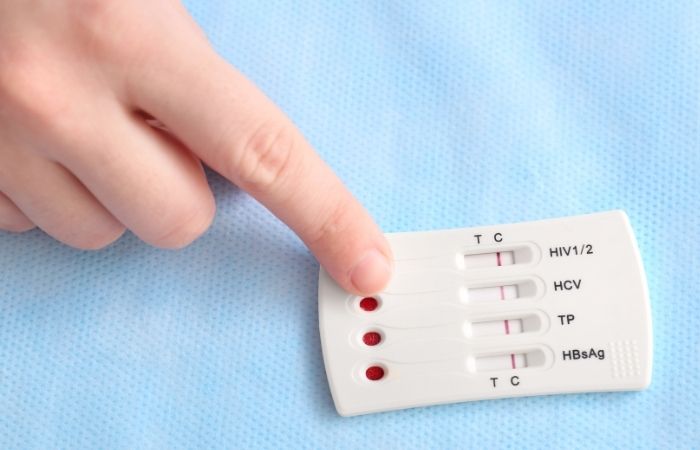
6. What’s the best STD test if I don’t know what I might have?
Go broad. A Combo STD Test Kit checks for multiple infections at once, HIV, chlamydia, gonorrhea, and more. It’s discreet, quick, and doesn’t require you to play guessing games with your symptoms.
7. Can I catch the same STD twice?
Yep. Especially with chlamydia or gonorrhea. You might treat it, feel better, and then get reinfected by the same partner if they never got tested. It’s the world’s least fun boomerang. Always loop your partner in. Always.
8. How private are these at-home tests, really?
Pretty much Fort Knox-level. Kits come in plain packaging, no neon "YOU MIGHT HAVE HERPES" tape. Results are viewable online, and no one knows unless you tell them. It's your body, your business.
9. When should I tell my partner I might’ve been exposed?
Sooner is better, but not in a panic text at 2AM. Be honest, be kind, and be direct. “Hey, something’s come up and I think we should both get tested.” Many services even offer anonymous partner alerts if saying it out loud feels impossible.
10. What if I’m scared to test?
That’s real. STD testing brings up shame, fear, trauma, all of it. But you deserve answers. And testing doesn’t mean something’s wrong with you, it means you care about your health. You’re being responsible, not reckless. That’s power, not weakness.
You’re Not Dirty, You’re Just Responsible
If you woke up today with a pit in your stomach and a question you can’t shake, you’re not broken. You’re human. Hookups, accidents, and curiosity happen, and so does risk. The difference is what you do next.
Testing isn’t shameful. It’s self-respect. It’s protecting future partners, your peace of mind, and your health. Whether you’re chasing symptoms, drowning in "what ifs," or just being cautious, getting tested is one of the most powerful things you can do for yourself.
How We Sourced This Article: We combined current guidance from leading medical organizations with peer-reviewed research and lived-experience reporting to make this guide practical, compassionate, and accurate. In total, around fifteen references informed the writing; below, we’ve highlighted six of the most relevant and reader-friendly sources.
Sources
1. About Sexually Transmitted Infections (STIs) – CDC
2. Getting Tested for STIs – CDC
3. Sexually Transmitted Infections (STIs) Fact Sheet – WHO
4. STDs: Symptoms and Causes – Mayo Clinic
About the Author
Dr. F. David, MD is a board-certified infectious disease specialist who focuses on preventing, diagnosing, and treating STIs. He combines clinical accuracy with a straightforward, sex-positive approach and is dedicated to making his work more accessible to readers in both urban and rural areas.
Reviewed by: A. Ramirez, NP | Last medically reviewed: January 2026
This article is for informational purposes and does not replace medical advice.







