At-Home HPV Test or Pap Smear? Here's How to Choose
Quick Answer: Men are not routinely tested for HPV unless visible symptoms like genital warts appear or specific high-risk screening is recommended. There is currently no approved general HPV screening test for asymptomatic men.
The Part No One Says Clearly Enough
Most sexually active people, including men, will contract HPV at some point in their lives. According to the CDC HPV Fact Sheet, nearly all sexually active individuals are exposed if they are not vaccinated. That statistic sounds terrifying until you understand the second half of the sentence: most infections clear on their own without causing problems.
But here’s where it gets complicated for men. There is no standard, FDA-approved routine HPV screening test for men like there is a Pap test for women. You can’t walk into most clinics and request a simple “HPV blood test.” In fact, HPV cannot be detected through blood at all. It lives in skin and mucosal tissue, not in your bloodstream.
This is why so many men leave doctor visits confused. They ask for an HPV test. The provider says there isn’t one. And suddenly it feels like medicine is shrugging at you.
People are also reading: 6‑in‑1 At‑Home STD Test Kit
Why There’s No Routine HPV Test for Men
This isn’t neglect. It’s biology and public health logistics colliding.
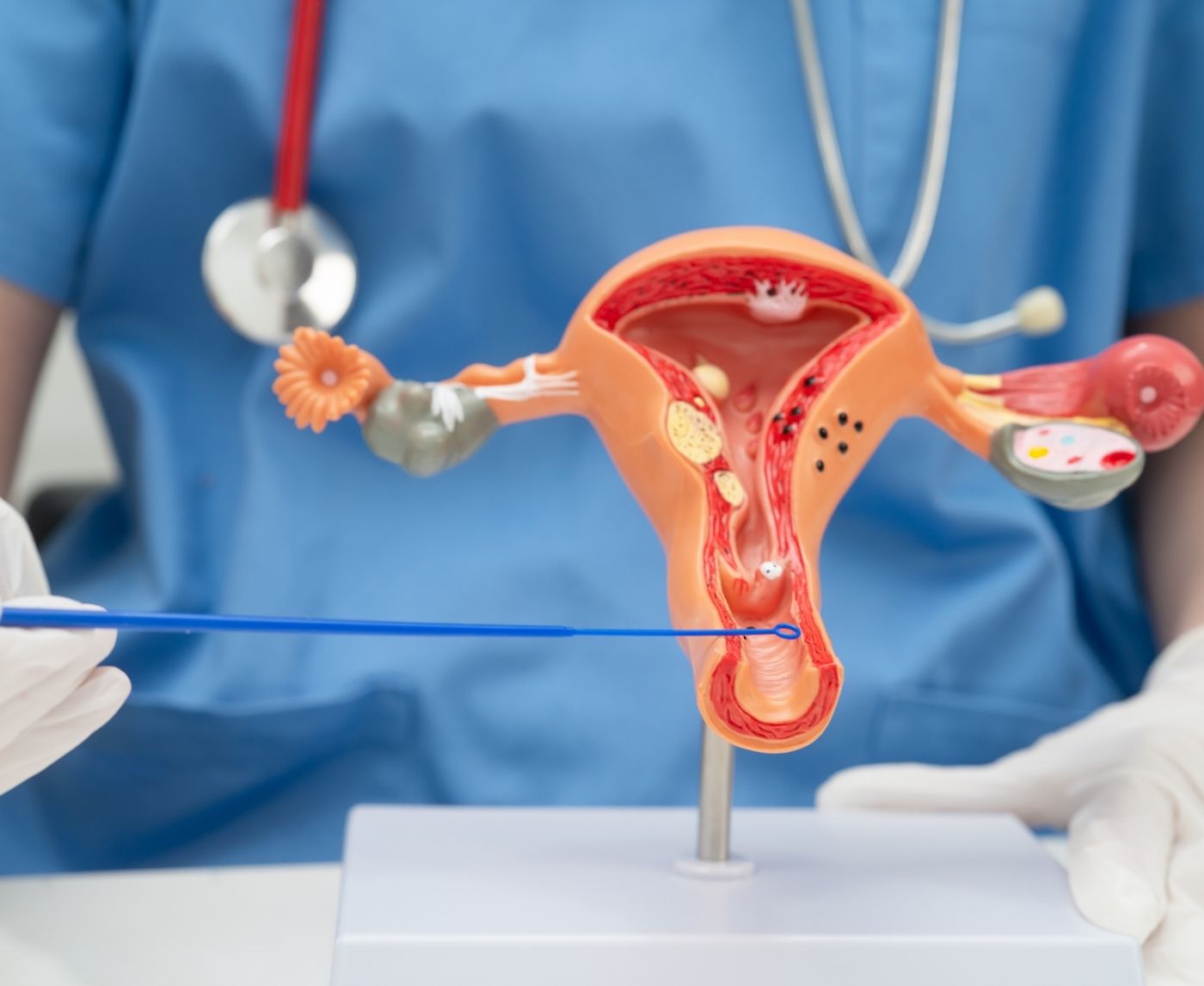
In women, HPV testing is tied to cervical cancer screening because the virus infects the cervix in a measurable, sample-friendly way. In men, HPV infects external genital skin, the anus, and sometimes the throat. There is no single sampling point that reliably detects all infections.
Research published in journals like Sexually Transmitted Diseases has shown that HPV detection in men varies widely depending on the anatomical site swabbed. A negative swab from one area does not guarantee absence elsewhere. That makes routine screening unreliable as a blanket approach.
In short: medicine doesn’t routinely test men because the results wouldn’t be consistently actionable. And giving people false reassurance can be more harmful than not testing at all.
What Testing Is Available for Men?
Now let’s get practical. While there’s no universal screening test for asymptomatic men, that doesn’t mean testing never happens.
If visible genital warts appear, a healthcare provider can diagnose low-risk HPV through visual examination. Sometimes a biopsy is done if the lesion looks atypical. For men at higher risk of anal cancer, including men who have sex with men (MSM) and individuals with HIV, some clinicians perform anal Pap tests to screen for precancerous changes.
Figure 1. Current HPV testing realities for men.
Notice what’s missing: there is no reliable urine test, no standard blood test, and no FDA-approved “HPV panel” for asymptomatic men.
“But My Partner Tested Positive. Should I Get Tested?”
This is where the anxiety spikes.
If your partner has HPV, the uncomfortable but honest answer is that you have likely already been exposed. The virus spreads through skin-to-skin sexual contact, not just penetration. Condoms reduce risk but do not eliminate it entirely because HPV can infect areas not covered by condoms.
So when men search “partner has HPV should I get tested,” what they’re really asking is: Am I in danger? Or sometimes: Did I cause this?
In most cases, testing is not recommended because management would not change. There is no antiviral treatment for HPV itself. Doctors treat visible warts or monitor abnormal cell changes. That’s it.
This doesn’t mean you do nothing. It means you shift the strategy from testing to prevention and awareness.
HPV Symptoms in Men: What to Watch For
Most men with HPV have no symptoms. That’s not comforting, but it is accurate.
When symptoms do appear, they typically look like small, flesh-colored or cauliflower-like bumps on the penis, scrotum, groin, or anus. These are caused by low-risk strains of HPV. High-risk strains, the ones linked to cancers, often produce no visible signs at all until much later.
Here’s a simplified breakdown:
Figure 2. Low-risk vs high-risk HPV strains in men.
According to the National Cancer Institute, high-risk HPV strains are linked to cancers of the penis, anus, and oropharynx. These outcomes are uncommon, but they are real, especially in unvaccinated individuals.
HPV Cancer Risk in Men: What’s Real and What’s Rare
When men search “HPV cancer risk in men,” it’s rarely casual curiosity. It’s usually fear. A late-night spiral. A throat that suddenly feels different. A small irritation that wasn’t there before.
Let’s steady this.
Most HPV infections clear naturally within one to two years, according to the Centers for Disease Control and Prevention. The immune system suppresses the virus quietly. No drama. No announcement.
But persistent high-risk HPV strains can, over time, cause cellular changes. In men, these cancers most commonly affect the anus, penis, and oropharynx (back of the throat, base of tongue, tonsils). The National Cancer Institute notes that HPV is responsible for the majority of oropharyngeal cancers in men.
That sounds heavy. So here’s context:
Figure 3. HPV-associated cancer risk landscape in men.
Notice a pattern? Screening exists only for select high-risk groups, and even then, it’s not universal. That’s part of why men feel stuck when they ask, “Can I just get tested?”
Can You Test for HPV at Home If You’re a Man?
This is where SEO meets reality.
There is currently no FDA-approved at-home HPV test for men that screens for all high-risk strains the way cervical HPV tests do for women. If you see websites advertising simple blood-based HPV detection for men, that’s misinformation. HPV is not detected in blood.
However, if you have visible genital warts, a clinician can diagnose them visually. And while you can’t directly test for HPV itself in most cases, you can test for other sexually transmitted infections that often coexist.
If you’re seeking broader clarity after an exposure, discreet panels are available through STD Test Kits. These test for infections like Chlamydia, Gonorrhea, Syphilis, and HIV, which are actually detectable through urine or blood.
Because sometimes the question isn’t just “Do I have HPV?” It’s “What else could this be?”
HPV Incubation Period in Men: Why Timing Feels So Vague
Another reason testing feels impossible is the incubation period.
HPV can take weeks, months, or even years to show visible signs. Genital warts may appear within weeks after exposure, but high-risk strains may remain silent indefinitely. There is no reliable “test at 14 days” timeline like there is for Chlamydia or HIV.
This is why men often Google “HPV incubation period men” and leave more confused than when they started. The virus doesn’t operate on a predictable countdown clock. And without a standardized screening test, there’s no defined “best testing date.”
What you can do instead is monitor your body and stay proactive with regular STD screening panels for other infections, especially after new partners.

People are also reading: Bleeding After Sex: Causes, STDs, and When It’s an Emergency
Can You Have HPV and Test Negative?
Yes, and this is critical to understand.
Even in research settings where penile or anal swabs are performed, HPV detection varies depending on the exact sampling site. A negative result from one area does not rule out infection elsewhere. This inconsistency is a major reason routine screening isn’t standard practice for asymptomatic men.
In other words: testing negative wouldn’t necessarily change your risk profile or management plan. That’s uncomfortable, but it’s honest.
What You Can Do Instead of Panicking
Let’s pivot from what’s unavailable to what’s actionable.
You can get vaccinated. The CDC recommends HPV vaccination for boys and young men, and catch-up vaccination is available into adulthood in many cases. The vaccine protects against the most dangerous high-risk strains and the common wart-causing strains.
You can use condoms consistently. They reduce, though do not eliminate, HPV transmission risk.
You can pay attention to persistent symptoms like unusual growths, bleeding, or throat pain lasting more than two weeks and seek medical evaluation promptly.
You can also reduce anxiety by testing for other STDs when appropriate. If you recently had a condom failure or new partner and your mind won’t quiet down, a comprehensive panel like the 6‑in‑1 At‑Home STD Test Kit can provide clarity on infections that are actually testable.
Peace of mind isn’t about testing for everything. It’s about testing for what can be tested, and protecting yourself where science gives us tools.
The Emotional Layer No One Talks About
Men rarely talk openly about HPV.
There’s a strange mix of guilt and helplessness that shows up in clinic rooms. “Did I give it to her?” “Does this mean I’m dirty?” “Why didn’t anyone tell me there’s no HPV test for men?”
Here’s the grounded truth: HPV is common. It spreads through normal sexual contact. Carrying it does not mean you were reckless. It means you’re human.
The goal isn’t perfection. The goal is informed choices.
Do Men Carry HPV Without Knowing It?
Yes. And this is the part that makes people uncomfortable.
When men search “do men carry HPV,” what they’re really asking is whether they can unknowingly pass something to someone they care about. The honest answer is that HPV is often asymptomatic in men. Most never develop visible warts. Most never feel a symptom. And yet, during that time, transmission is possible.
According to data referenced by the World Health Organization, HPV is one of the most common viral infections of the reproductive tract. In men, it frequently clears without ever being detected. But “clears” doesn’t mean it never existed. It just means your immune system handled it.
This is why testing doesn’t function the way people want it to. There is no moment where you can definitively declare yourself permanently HPV-free. The virus behaves differently from infections like Chlamydia or Gonorrhea, which can be detected and treated directly.
How HPV Spreads (And What Condoms Actually Do)
HPV spreads through skin-to-skin contact during vaginal, anal, or oral sex. Penetration is not required. Ejaculation is not required. This surprises many people.
Condoms significantly reduce transmission risk but do not eliminate it entirely. That’s because HPV can infect areas not covered by a condom, including the base of the penis, scrotum, or surrounding groin tissue.
Here’s what research consistently shows:
Figure 4. HPV prevention strategies and their limitations.
The point isn’t that condoms “don’t work.” They absolutely reduce risk and should be used. The point is that HPV transmission isn’t binary. It’s probabilistic.
“She Tested Positive. I Feel Responsible.”
Let’s put a human voice in this.
Marcus, 29, got a text from his girlfriend after her routine gynecological exam. Her Pap test showed high-risk HPV. She was calm. He was spiraling.
“I kept thinking, I must’ve given it to her. I felt sick about it.”
He searched how men get tested for HPV. He booked a doctor’s appointment. The physician explained there was no routine screening test for him. Marcus left frustrated, feeling like he’d failed some invisible health exam.
But here’s what actually happened: HPV is common. Either partner could have carried it silently for years. There is no reliable way to determine origin. Blame doesn’t apply because timelines are rarely clear.
This is where education matters more than testing. Understanding prevalence reduces shame. According to the CDC, most sexually active people are exposed at some point. That statistic reframes everything.
HPV vs. Herpes: Why Men Confuse the Two
Another common anxiety spiral involves symptom confusion.
Men often Google “HPV vs herpes in men” after noticing a bump. The two viruses are different. Herpes typically causes painful blisters that break open and crust over. HPV-related genital warts are usually painless, raised, and cauliflower-like in appearance.
But not every bump is either virus. Razor burn, ingrown hairs, molluscum contagiosum, and benign skin tags can mimic STDs. This is why visual self-diagnosis through internet images often increases anxiety rather than reducing it.
However, if you are not sure, it is always possible to get the lesions checked by a medical professional. Additionally, if you are worried about other potential exposures after a recent encounter, it is possible to get comprehensive screening to rule out other testable infections. When considering your options with STD Test Kits, it is possible to discreetly test for common STDs with clear diagnostic pathways.
Why Medicine Focuses on Vaccination Instead of Testing
This is strategic, not dismissive.
Public health authorities prioritize HPV vaccination because preventing infection in the first place reduces cancer risk more effectively than attempting widespread screening in men. The current vaccines protect against the strains most commonly associated with genital warts and cancer.
Vaccination is recommended routinely for adolescents and is available for many adults up to age 45 depending on individual circumstances. If you’re searching “should men get HPV vaccine,” the short answer is yes, especially if you were not vaccinated earlier.
Vaccination does not treat existing infection, but it can protect against strains you have not yet encountered.
The Bigger Sexual Health Picture
Here’s something rarely discussed: HPV often exists in a broader sexual health context.
If you’re worried about HPV after a new partner, it may also be wise to screen for other infections with defined window periods and treatment options. Syphilis, HIV, Chlamydia, and Gonorrhea have clear testing protocols.
The reason doctors sometimes redirect men toward broader STD screening isn’t avoidance. It’s prioritization. They focus on infections where early detection changes outcomes immediately.
If your anxiety is coming from a recent exposure and you want structured reassurance, testing for those infections can offer clarity while you monitor for HPV-related symptoms.

People are also reading: HIV From Oral Sex: Is Giving or Receiving Riskier?
If You Can’t Test Routinely, What Should You Actually Do?
Let’s bring this home.
If you came here asking “can men be tested for HPV,” what you were really asking was: Am I safe? Did I miss something? Is there something hiding in my body I can’t see?
Here’s the grounded answer. There is no routine screening test for asymptomatic men. But there is a strategy.
That strategy includes vaccination if eligible, consistent condom use, awareness of persistent symptoms, and regular STD screening for infections that can be detected and treated early. It means not waiting months with unexplained growths or bleeding. It means not spiraling in silence.
It also means understanding that HPV is common. So common that exposure is considered a normal part of sexual life for most adults.
If you want broader reassurance after a new partner or condom failure, consider a comprehensive panel like the 8‑in‑1 Complete At-Home STD Test Kit. While it does not test for HPV directly, it screens for other common infections that do have clear diagnostic answers. Sometimes clarity in one area quiets fear in another.
FAQs
1. So… can men actually be tested for HPV or is that a myth?
It’s not a myth, it’s just limited. If you have visible genital warts, a clinician can diagnose those. If you’re in a higher-risk group, like men who have sex with men or individuals living with HIV, anal screening may be offered. But if you’re symptom-free and part of the general population, there’s no routine screening test doctors can run just for reassurance.
2. Why can women get tested but men can’t?
It feels unfair, right? Women are screened because HPV can infect the cervix in a way that’s measurable and predictable. There’s a clear sampling site. In men, the virus can live on different areas of skin, and swabbing one spot doesn’t reliably tell the whole story. Medicine isn’t ignoring men, it just doesn’t have a consistent testing target.
3. If my partner tested positive, does that automatically mean I gave it to her?
No. And this is where guilt loves to sneak in. HPV can stay dormant for years before showing up on a screening test. Either partner could have carried it silently. There is almost never a clear “source.” Blame doesn’t help. Information does.
4. Can I ask my doctor to test me anyway?
You can always ask. But most providers will explain that routine testing in asymptomatic men isn’t recommended because the result wouldn’t change your care plan. That can feel dismissive, but it’s actually about avoiding misleading or incomplete results.
5. What if I notice a bump and I’m freaking out?
First: breathe. Not every bump is HPV. Ingrown hairs, skin tags, friction irritation, they’re common. HPV warts are usually painless, flesh-colored, and raised. If something sticks around longer than two weeks, grows, bleeds, or changes, get it looked at. A quick exam can bring more peace than hours of scrolling photos online.
6. Can men get cancer from HPV?
Yes, but let’s get real here. Most HPV infections will resolve on their own. Persistent high-risk HPV infections can lead to anal, penile, and throat cancers in unvaccinated men. The operative word here is persistent. So, vaccination and awareness of symptoms are more important than screening itself.
7. If there’s no HPV test, how do I protect myself?
Vaccination is the biggest move. Condoms lower transmission risk. And regular STD testing for other infections, the ones that are testable, keeps your overall sexual health in check. Protection is layered. It’s not one single magic lab result.
8. Is there an at-home HPV test for men I can order?
Not a reliable, FDA-approved one for general screening. If you see ads promising blood-based HPV detection, that’s a red flag. However, you can test at home for other STDs that often cause similar anxiety after exposure. Sometimes ruling out what’s testable helps calm what isn’t.
9. How long would it take for HPV symptoms to show up?
It varies wildly. Some genital warts appear within weeks. High-risk strains may never cause visible symptoms at all. That unpredictability is exactly why there isn’t a “test on day 10” rule like there is for other infections.
10. If most people get HPV, why does it feel so scary?
Because we talk about it in whispers. Because it’s tied to sex. Because no one teaches men what to expect. But medically speaking, HPV exposure is incredibly common. What matters is how you respond, with prevention, awareness, and zero shame.
How We Sourced This Article: This guide draws from current recommendations by the Centers for Disease Control and Prevention (CDC), the World Health Organization (WHO), and the National Cancer Institute, alongside peer-reviewed research on HPV prevalence and detection in men. We reviewed approximately fifteen medical and public health references to ensure accuracy, clarity, and relevance. Only the most authoritative and reader-accessible sources are listed below.
Sources
1. World Health Organization – HPV Fact Sheet
2. About Genital HPV Infection | CDC
3. Chapter 11: Human Papillomavirus | CDC Pink Book
4. Human Papillomavirus Vaccination: Recommendations of the ACIP | CDC/MMWR
5. HPV and HPV Testing | American Cancer Society
About the Author
Dr. F. David, MD is a board-certified infectious disease specialist focused on STI prevention, diagnosis, and treatment. He combines clinical precision with a stigma-free, sex-positive approach to sexual health education.
Reviewed by: Michael R. Kline, MD | Last medically reviewed: February 2026
This article is for informational purposes and does not replace medical advice.