When the STD Test Says “Negative” But Your Body Says “Something’s Wrong”
Quick Answer: Oral sex itself doesn’t directly cause sinus infections, but it can expose you to throat-based STDs like gonorrhea, chlamydia, or syphilis, some of which cause symptoms that feel like sinus congestion, sore throat, or postnasal drip.
“I Gave Head and Now I Feel Sick”, You’re Not Alone
Jordan, 26, woke up three days after a one-night stand with a scratchy throat and sinus pressure. “I didn’t even kiss him, just oral,” he said. “But my whole head feels off. Could I have caught something?”
This scenario is incredibly common, and there are a few reasons for it. First, oral sex doesn’t come with the same cultural “risk warning” as unprotected vaginal or anal sex, even though it can still transmit several STDs. Second, the throat and sinuses are physically connected. That means any irritation, infection, or inflammation in your pharynx (the back of your throat) can feel like a sinus issue.
So if you’re dealing with post-oral symptoms, especially sinus pressure, sore throat, or stuffy nose, it’s worth asking: is this a cold, or could it be something else?

People are also reading: Can You Go to Urgent Care for STD Testing?
Can Oral Sex Trigger a Sinus Infection?
In short, no. Viruses, bacteria, or allergens, not sexual activity, are the most common causes of sinus infections (also known as sinusitis). But oral sex can bring new bacteria into the mouth and throat, which can lead to localized inflammation or infections, especially if your immune system is already weak.
According to the CDC, oral sex is a known transmission route for several STDs that can affect the throat, including:
Figure 1. Throat STDs and sinus-mimicking symptoms. While these infections don’t cause sinusitis per se, they can lead to discomfort that feels very similar, especially early on.
Why Oral Sex Symptoms Can Feel Like a Sinus Infection
Your sinuses and throat share a lot of real estate. The back of your nasal cavity (called the nasopharynx) connects directly to the upper throat. When an STD like gonorrhea or syphilis infects this area, it can create swelling, pressure, or even drainage that resembles postnasal drip or a sinus infection.
Even beyond infections, oral sex involves contact with mucus membranes. If there’s any minor trauma, allergic reaction (e.g., to lube or latex), or microbiome disruption, it can trigger local inflammation. This leads to symptoms like:
- Sore throat or scratchiness
- Pressure behind the eyes or forehead
- Fatigue or mild body aches
- Congestion or stuffy nose
These symptoms can last a few hours or linger for days, and they don’t automatically mean you have an STD. But if they don’t improve or seem to get worse, it’s time to consider testing.
When to Test After Giving or Receiving Oral Sex
Not all throat infections show up immediately, especially if they’re caused by STDs. Most bacterial STDs that infect the throat have a window period, which is the time between exposure and when the infection becomes detectable on a test. Testing too soon can lead to false negatives, leaving you falsely reassured while the infection spreads silently.
Here's what the testing windows look like for oral exposure:
Figure 2. Window periods for oral STDs. Waiting for the optimal test window helps ensure accurate results.
If you’ve already tested but symptoms persist, or if your result was negative within the first week of exposure, consider retesting at the optimal time. Accuracy improves significantly after the first 10–14 days for most bacterial infections.
For example, this Chlamydia test kit can detect infections in swab samples, ideal for genital or oral exposure. Just be sure to follow proper sample collection instructions to avoid false negatives.
“It Was Just a Throat Thing… Until It Wasn’t”
Lina, 22, thought she had a seasonal allergy flare-up after giving oral sex to a casual partner. “My sinuses were acting up, and I had this sore throat that wouldn’t go away,” she said. “I figured it was just the changing weather.”
She took cold medicine, drank tea, and waited it out. By the second week, her throat still felt raw, and her lymph nodes were swollen. “I finally went in for testing,” Lina recalled. “Turns out I had throat gonorrhea.”
Throat gonorrhea often causes no symptoms at all. When it does, it can mimic allergies, mild viral infections, or sinus issues. Left untreated, it can contribute to other infections, and increase the risk of passing it on during future oral sex or kissing.
Stories like Lina’s are why health experts recommend testing even when symptoms seem “mild” or unrelated to sex. Throat STDs are underdiagnosed not because they’re rare, but because people don’t associate them with things like sinus pressure, postnasal drip, or a lingering cough.
Not All Post-Oral Sex Illnesses Are STDs, But Some Are
It’s entirely possible to catch a cold, get a sinus infection, or have minor throat irritation after oral sex without any STD being involved. But here’s what makes it tricky: STDs that infect the throat often present with exactly those symptoms. So while your body might just be reacting to friction, allergens, or unrelated viruses, there’s also a possibility you’ve picked up something from your partner’s genital, oral, or rectal microbiome.
Here are a few potential causes of post-oral sinus-like symptoms, and how to think about them:
Figure 3. Symptom-by-symptom breakdown of what’s likely, and when to test.
Why Symptoms Sometimes Return, and When to Retest
Maybe your sore throat disappeared after two days. You stopped worrying, chalked it up to dryness or allergies. Then, out of nowhere, the tightness came back, or you felt a new kind of pressure behind your eyes. Should you test again?
Yes, because symptoms that come and go could mean the infection never left. Some oral STDs like gonorrhea or chlamydia can temporarily ease up if your immune system fights them off partially. But that doesn’t mean they’re gone. These infections can linger silently, especially in the throat, where they often don’t trigger a strong response.
If you’ve already tested once and it was early (within the first 7 days after exposure), here’s when to consider retesting:
- 10–14 days after exposure for most throat-based bacterial STDs
- 6+ weeks if concerned about syphilis, which takes longer to show up
- Immediately if symptoms worsen or change (e.g., new lymph node swelling, pain when swallowing)
We often hear stories like this:
Jay, 30, tested negative for throat STDs at a local clinic on day four after a hookup. “My symptoms were bad, like, real sinus pressure and fatigue, but the nurse said my tests were clear,” he said. “Then two weeks later, I had swollen tonsils and low fever. I got retested, and it was gonorrhea after all.”

People are also reading: Hooked Up and Wiped Out? Fatigue After Sex Might Mean More Than Pleasure
Privacy, Discretion, and What Support Looks Like
If you're feeling embarrassed, overwhelmed, or just want to handle this quietly, you’re not alone. Many people seek out at-home testing because they don't want to explain symptoms that feel “silly” or “small.” But there’s nothing small about taking care of your health.
All at-home STD test kits from STD Test Kits ship in unmarked packaging, no company name, no indication of what’s inside. Results stay private. No insurance billing. No awkward pharmacy pickups. Just you, your sample, and your next step.
Even better: most kits offer fast shipping and simple instructions. You can test before a trip, after a hookup, or while crashing at a friend’s place. Wherever you are, peace of mind doesn’t have to wait.
What If It’s Positive?
First of all, breathe. Most oral STDs are easily treatable with a short course of antibiotics. You’re not doomed. You’re not dirty. And you’re not alone.
Start by confirming the result. If you used an at-home kit, follow up with a telehealth provider or clinic if needed. A positive throat swab for gonorrhea or chlamydia usually leads to a one-time dose or short prescription. If it’s syphilis, treatment is still straightforward, though follow-up is key.
Let’s make this real:
Chris, 35, got his positive result while parked outside a coffee shop. “I felt like the world was closing in,” he said. “But I took a deep breath, messaged my partner, and called a telehealth clinic that afternoon. I had meds in hand within 24 hours. It was way less dramatic than I thought.”
Testing positive doesn’t mean you did something wrong, it means you did something right. You found out. You took action. That’s more than most people ever do.
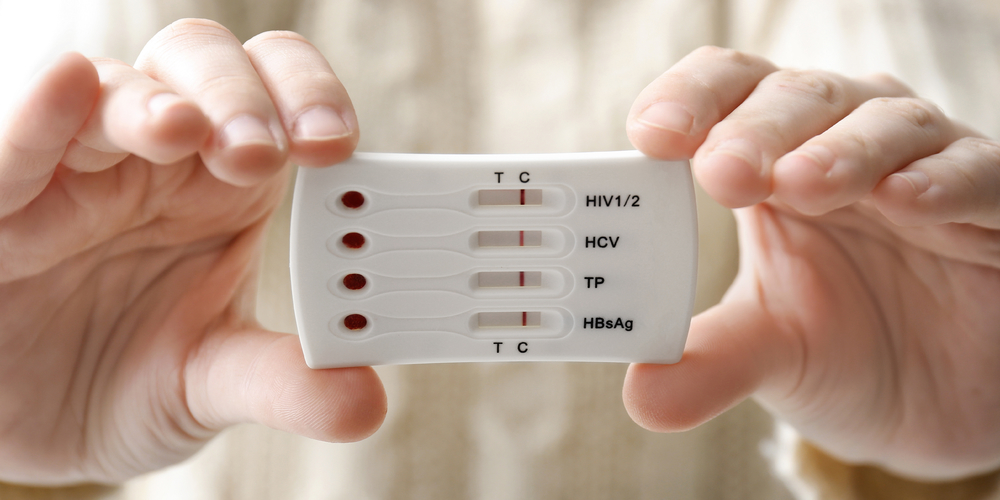
Whether you need to treat, retest, or just know you’re clear, our combo STD home test kit is designed to meet you exactly where you are, private, fast, and no judgment.
FAQs
1. Can you really get a sinus infection from oral sex?
Not in the direct, textbook way. A true sinus infection, where the nasal cavities fill with gunk from bacteria or a virus, usually comes from a cold, allergies, or respiratory bugs. But here’s the twist: if you give oral and suddenly have sinus-like symptoms, it could be a throat STD stirring up inflammation that feels eerily similar. So yeah, the timing isn’t always a coincidence.
2. My throat hurts a day after giving head, should I be worried?
Maybe, but not automatically. A sore throat could come from friction (especially if things got... enthusiastic), dryness, or even allergies. But if it lingers more than 2–3 days, or you start feeling swollen glands, fatigue, or sinus pressure, don’t brush it off. Some STDs like throat gonorrhea or syphilis start subtle. When in doubt, test.
3. What kind of STD can live in your throat?
The big players are gonorrhea, chlamydia, syphilis, and sometimes herpes. HPV can also infect the throat, though it’s usually silent unless it causes warts or lesions. The tricky part? Many throat infections have zero symptoms, which is why people pass them along without knowing.
4. How soon after oral sex can I get tested?
You can test for most bacterial infections (like gonorrhea and chlamydia) around 7 to 14 days after exposure. Testing too early might miss the infection. If you’re already having symptoms, a throat swab can often detect what’s up sooner, but keep in mind, you may still need a retest to confirm.
5. Can a cold mask a throat STD?
Yep, and that’s part of the problem. Both can cause sore throat, postnasal drip, mild fever, and fatigue. If you’re recovering from a cold and things don’t improve… or feel different than usual (like tender lymph nodes or pain when swallowing), it’s worth checking for STDs, especially if you’ve had recent oral contact.
6. Do I need to see a doctor to get a throat STD test?
Not necessarily. At-home throat swab kits exist (and yes, they’re legit). You can swab yourself, mail it in, and get results in a few days. Just make sure the kit is designed for oral testing, not all are.
7. If it goes away on its own, is it still a problem?
Even if your sore throat fades, the infection might not be gone. Some STDs calm down temporarily before flaring up again, or they just hang out quietly, waiting to be passed on. A symptom disappearing doesn’t mean you’re in the clear. Test to know, not to guess.
8. Is throat gonorrhea serious?
It can be. Even if you feel fine, untreated gonorrhea in the throat can cause inflammation, make you more likely to get or give other infections, and become antibiotic-resistant if left too long. The fix is simple (usually one round of antibiotics), but only if you catch it.
9. Can I pass a throat STD to someone just by kissing?
Possibly, but it depends on the infection. Herpes and syphilis are most likely to spread via kissing, especially if there are open sores. Gonorrhea or chlamydia are less likely, but not impossible. If you’re actively infected and swapping spit, there’s a chance.
10. Should I tell my partner if I tested positive for something oral?
Yes, and it doesn’t have to be scary. Think of it as health care, not a confession. You’re helping them stay safe, and there are even anonymous notification services if talking face-to-face feels impossible. Whatever you do, don’t ghost the convo. Ghost the infection instead.
You Deserve Real Answers, Not Panic
If your body is sending you mixed signals after a hookup, don’t let fear make the decisions. Whether it’s a harmless sore throat or something that needs treatment, the only way to know for sure is to get tested. And the good news? You don’t have to leave your house to do it.
This at-home combo test kit checks for the most common STDs in multiple areas of the body, including oral exposure, with clear instructions and fast results.
Your body is talking. Let’s stop guessing, and start listening.
How We Sourced This Article: We combined current guidance from leading medical organizations with peer-reviewed research and lived-experience reporting to make this guide practical, compassionate, and accurate. In total, around fifteen references informed the writing; below, we’ve highlighted some of the most relevant and reader-friendly sources.
Sources
1. WHO – Sexually Transmitted Infections Fact Sheet
2. Medical News Today – Chlamydia in the Throat
3. About STI Risk and Oral Sex – CDC
5. Sexually Transmitted Infections Treatment Guidelines, 2021 – CDC
About the Author
Dr. F. David, MD is a board-certified infectious disease specialist who focuses on preventing, diagnosing, and treating STIs. He combines clinical accuracy with a straightforward, sex-positive approach and is dedicated to making his work more accessible to readers in both urban and rural areas.
Reviewed by: A. Chen, NP, MPH | Last medically reviewed: January 2026
This article is for informational purposes and does not replace medical advice.