When the STD Test Says “Negative” But Your Body Says “Something’s Wrong”
Quick Answer: Fishy smell after sex is most often caused by Bacterial Vaginosis (BV) or a temporary vaginal pH shift from semen. It can sometimes signal Trichomoniasis, but most STIs like chlamydia and gonorrhea do not cause a strong odor on their own. Testing is recommended if the smell lasts more than 2–3 days, comes with unusual discharge, or keeps recurring.
The 1AM Bathroom Moment: What’s Actually Happening
Erika, 26, noticed it first after a new partner. “It wasn’t there before we had sex,” she told me. “It was fine all day. Then the next morning I smelled… off. Like fish. I immediately thought, ‘He gave me something.’”
That reaction is incredibly common. Odor feels like proof. Like evidence. But here’s what most people don’t know: semen is alkaline. The vagina is acidic. And when those two meet, chemistry happens.
The normal vaginal pH sits between about 3.8 and 4.5. That acidity is protective. It keeps healthy Lactobacillus bacteria dominant and suppresses overgrowth of other organisms. Semen, however, has a pH around 7.2 to 8.0. It’s designed to temporarily neutralize vaginal acidity so sperm can survive.
That temporary shift can change odor within hours. Not because you’re infected. Because the environment shifted.
But, and this matters, if the smell is distinctly “fishy,” especially strong after sex, that’s when we start thinking about Bacterial Vaginosis (BV).

People are also reading: Swollen Lymph Nodes in Groin: STD or Something Else?
When It’s Just pH, and When It’s Bacterial Vaginosis
A temporary pH change after condomless sex can cause a mild, slightly sour or musky scent that fades within a day. It usually does not come with heavy discharge, itching, or irritation. It feels like your body recalibrates on its own.
Bacterial Vaginosis is different. BV happens when the protective lactobacilli decrease and other anaerobic bacteria overgrow. One of the byproducts of that bacterial shift is amines, compounds that smell distinctly fishy. And semen can amplify that smell because alkaline fluid makes those amines more volatile.
This is why many people say, “It only smells fishy after sex.” The BV may already be present at low levels, but intercourse makes the odor obvious.
Figure 1. Differences between temporary semen-related pH changes and Bacterial Vaginosis patterns.
Here’s the key: BV is not technically classified as a traditional STD. But sexual activity, especially new or multiple partners, can increase risk because it alters the vaginal microbiome.
That nuance matters. Because smelling different after sex does not automatically mean someone “gave you an STI.” Sometimes, your microbiome just shifted.
But Could It Be an STD?
This is the fear spiral part. You search “STD that smells fishy.” You brace yourself.
Chlamydia and Gonorrhea, two of the most common STIs, don't usually smell very fishy. They often make you feel like you have to pee, have pelvic pain, or have strange discharge without that smell.
There is one infection that can cause odor similar to BV: Trichomoniasis.
Trichomoniasis is caused by a parasite and can lead to a fishy or unpleasant odor, often paired with frothy yellow-green discharge and irritation. However, many cases are mild or asymptomatic.
The difference between BV and Trichomoniasis is not something you can reliably smell your way through. Testing is the only way to know for sure.
Figure 2. Odor patterns across BV and common sexually transmitted infections.
If odor is the only symptom, and especially if it spikes right after condomless sex, BV or pH shift are statistically more likely than chlamydia or gonorrhea. But if the smell persists more than a few days, recurs frequently, or comes with irritation or unusual discharge, testing becomes smart, not paranoid.
The Science Part (Without the Boring Lecture)
Your vaginal microbiome is an ecosystem. When lactobacilli dominate, they produce lactic acid and hydrogen peroxide that keep pH low and pathogens suppressed. When that balance shifts, because of semen, douching, antibiotics, hormonal changes, or new sexual partners, anaerobic bacteria can overgrow.
Those bacteria produce amines. Amines smell like fish. Add alkaline semen, and those amines volatilize, meaning they evaporate into the air more easily, making the smell sharper after sex.
This is called the “whiff test” in clinical settings. When potassium hydroxide is added to a vaginal sample, the fishy odor intensifies if BV is present. Semen essentially does a similar thing temporarily.
So… When Should You Actually Test?
If the smell disappears within 24 hours and doesn’t come back, you likely experienced a simple pH fluctuation. No treatment needed.
If the odor lasts more than 2–3 days, comes with thin discharge, or keeps recurring after sex, testing for Bacterial Vaginosis is appropriate. If irritation, burning, or unusual colored discharge are present, testing for Trichomoniasis, Chlamydia, and Gonorrhea should be considered as well.
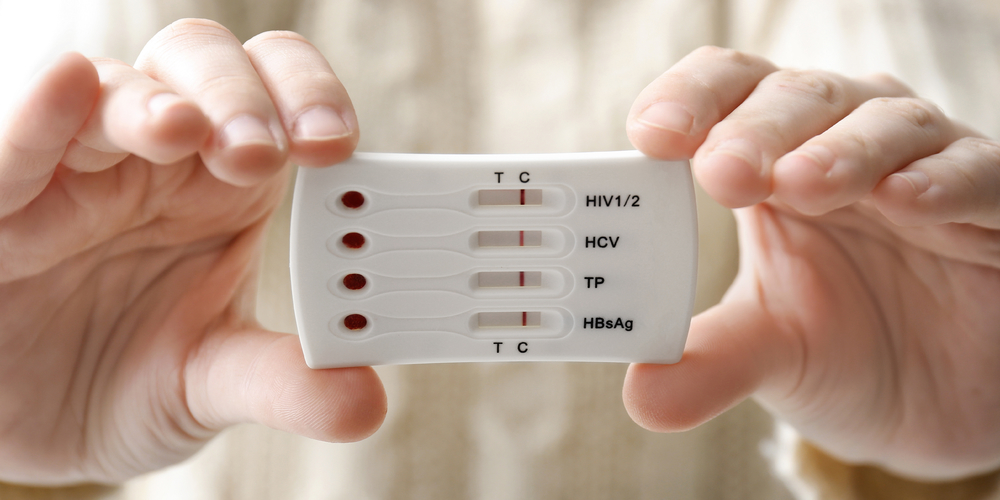
This is where control comes back into your hands. You don’t have to spiral or wait for a clinic appointment weeks out. You can explore discreet options at STD Test Kits, including combination panels that check for common STIs at home.
If odor and discharge are your main concerns, a multi-panel test that includes trichomoniasis alongside chlamydia and gonorrhea can offer clarity quickly and privately.
Why BV Comes Back After Sex (And Why It’s Not Your Fault)
Let’s talk about the pattern a lot of people are scared to admit.
You treat the Bacterial Vaginosis. The smell goes away. You feel normal again. Then you have sex, sometimes with the same partner, sometimes a new one, and within 24 to 72 hours, the fishy smell creeps back.
Lena, 31, told me, “I started thinking I was allergic to my boyfriend. Every time we had sex, it came back. I felt broken.”
You’re not broken. And you’re definitely not allergic to him.
BV recurrence is common. Studies show that up to 50% of people experience recurrence within 6 to 12 months. That’s not because you’re “dirty.” It’s because the vaginal microbiome is delicate, and semen repeatedly shifts its pH.
Semen doesn’t “infect” you. It changes the environment. If your lactobacilli levels are already borderline low, repeated alkaline exposure can give anaerobic bacteria another chance to overgrow.
This is why condom use sometimes reduces BV recurrence. It’s not about morality. It’s about chemistry.
Does Semen Cause BV , Or Just Trigger It?
This is where nuance matters.
Semen does not contain BV bacteria in the way an STD contains a specific pathogen. BV is a dysbiosis, an imbalance of bacteria that are already present in the vagina. But semen’s alkaline pH can disrupt the acidic environment that normally keeps those bacteria in check.
Think of it like this: the bacteria are already in the room. Semen just opens the windows and turns on a fan.
For some people, that temporary shift resolves quickly. For others, especially if they’ve recently taken antibiotics, douched, experienced hormonal changes, or had a new partner, that shift can tip into symptomatic BV.
That’s not about blame. It’s about vulnerability in the ecosystem.
Recurring Fishy Smell With One Specific Partner
This is the part that gets emotionally messy.
You might notice that the odor only happens with one person. And that can spiral into suspicion fast.
Here’s what’s more likely: every person has a unique microbiome. When two microbiomes interact repeatedly, they influence each other. There’s growing evidence that sexual partners can exchange bacteria that subtly affect vaginal balance, even when neither person has an STI.
That doesn’t automatically mean someone is cheating. It doesn’t automatically mean someone has Trichomoniasis or another infection. It can simply mean your microbiome reacts differently to that partner’s semen or genital flora.
If BV keeps recurring with the same partner, both of you may benefit from evaluation. While routine male treatment for BV isn’t standard, persistent recurrence sometimes warrants clinical discussion.

People are also reading: Pain During Sex STD Warning Signs People Ignore
How Long Should a Fishy Smell Last?
This question is huge for anxiety.
If the smell fades within 24 hours and doesn’t return, it was likely a temporary pH shift. No infection. No treatment required.
If it lasts 2–3 days or more, especially with thin gray or white discharge, that strongly points toward Bacterial Vaginosis.
If odor is paired with irritation, burning during urination, or frothy yellow-green discharge, testing for Trichomoniasis becomes important.
Here’s a simple timing breakdown:
Figure 3. Duration-based decision guidance for post-sex fishy odor.
What Not To Do (Even Though You’re Tempted)
When people notice a fishy smell, they often panic-clean.
Douching. Scented washes. Hydrogen peroxide rinses. Apple cider vinegar baths. TikTok hacks.
These often make things worse. Douching raises pH further and disrupts protective lactobacilli. Scented products can irritate tissue and prolong imbalance. The vagina is self-cleaning. Over-correcting can extend the problem.
If BV is present, it usually requires antibiotics like metronidazole or clindamycin prescribed by a clinician. Over-the-counter “odor masking” products don’t treat the underlying imbalance.
Testing: What, When, and How
If you’re not sure whether it’s BV or an STD, testing helps take the guesswork out of the situation.
To test for BV, pH testing, microscopic evaluation, or molecular testing can be done. To test for STIs such as Trichomoniasis, Chlamydia, and Gonorrhea, NAATs are highly sensitive.
Time is relevant if the exposure was recent. For most bacterial STIs, testing can be done reliably within 7 to 14 days of exposure. Testing for Trichomoniasis can be done within a week. Testing too soon can give false reassurance.
If the smell is your only symptom and it’s persistent, a combination panel offers clarity without having to guess which infection to test for.
You can order discreet testing options directly from STD Test Kits. If you want broader coverage, the 6‑in‑1 At‑Home STD Test Kit checks for multiple common infections in one panel.
Testing isn’t an accusation. It’s data.
Clinic vs At-Home Testing: Which Makes Sense?
If you have severe pain, fever, pelvic tenderness, or pregnancy issues, you should seek a clinic as soon as you can. These are not “wait and see” symptoms.
If you are mostly experiencing odor and discharge and want to have privacy, you can use an at-home testing kit. These can give you answers fast. Lab kits sent by mail can give you high accuracy while allowing for discreet shipping. Rapid tests give you quick answers but may require further testing depending on the infection.
The choice is based on your symptoms, time constraints, and personal comfort. The point is to get answers, not to punish.
BV, Yeast, or Something Else? The Smell Confusion Trap
Let’s clear up one of the biggest misconceptions on the internet: yeast infections usually do not smell fishy.
Aria, 24, told me, “I assumed it was yeast because I’ve had that before. But this time it smelled… different. Strong. Almost metallic-fishy. I kept using antifungal cream and it didn’t help.”
That’s because yeast infections typically cause thick, white, cottage cheese–like discharge and intense itching, but minimal odor. If there’s a smell, it’s often mild or bread-like, not fishy.
When the odor is distinctly fishy, especially stronger after sex, Bacterial Vaginosis is statistically more likely than yeast.
Here’s a direct comparison:
Figure 4. Odor and symptom comparison: BV vs yeast vs trichomoniasis.
If antifungal treatment doesn’t improve symptoms within a few days, reassessment is essential. Treating the wrong condition can prolong imbalance and delay real care.
Can Oral Sex Cause a Fishy Smell?
This is a question people whisper.
Oral sex introduces oral bacteria into the vaginal ecosystem. While this doesn’t automatically cause Bacterial Vaginosis, it can shift the microbiome slightly, especially if your balance is already fragile.
Saliva has a higher pH than the vagina. So yes, theoretically, oral sex can temporarily alter vaginal acidity. But persistent fishy odor after oral sex usually still points toward BV rather than a typical STI.
If you experience new discharge, irritation, or symptoms after oral sex with a new partner, testing for Chlamydia, Gonorrhea, and Trichomoniasis may still be reasonable, particularly if the encounter was unprotected.
Again: odor alone is not a reliable STI diagnostic tool. Testing is.
Pregnancy and Fishy Odor After Sex
Pregnancy causes changes in hormone levels that alter the discharge and microbial flora in the vagina. Estrogen level changes may affect lactobacillus levels, making a woman more susceptible to BV.
Vaginal discharge with a fishy smell during pregnancy requires attention and should not be taken lightly. Untreated BV in pregnant women may lead to preterm labor.
Do not take any medication to treat a fishy smell during pregnancy without medical attention. Proper diagnosis is necessary.
What Happens If BV Is Left Untreated?
Sometimes people wait it out. Sometimes it resolves. But persistent untreated BV can increase susceptibility to acquiring STIs, including HIV. It can also raise the risk of pelvic inflammatory disease when other infections are present.
The reason is biological: when lactobacilli levels drop, protective acidity drops too. That makes the vaginal lining more vulnerable to pathogen entry.
This isn’t about fear. It’s about risk context.
If odor persists beyond several days or recurs frequently, getting tested is proactive, not dramatic.
Long-Term Microbiome Care
If BV keeps recurring after sex, prevention strategies can help reduce episodes:
Using condoms to reduce alkaline exposure. Avoiding douching or scented washes. Completing full antibiotic courses when prescribed. Following up if recurrence becomes frequent.
Some clinicians discuss probiotics containing lactobacillus strains, though evidence is still evolving. The key is restoring acidic balance, not sterilizing the vagina.
Your body is designed to regulate itself. Sometimes it just needs a little help, not punishment.
People are also reading: Anal Itching After Sex? Here’s What It Could Mean
FAQs
1. Is a fishy smell during sex always Bacterial Vaginosis?
Nope. It’s possible that the pH in your vagina was just adjusting to the presence of semen. If the smell goes away in a day or two without reappearing, your body was probably just adjusting to the new pH. But if the smell persists for an extended period or reoccurs every time you have sex, Bacterial Vaginosis takes priority on the list.
2. Why does the smell seem worse during or after sex?
It’s chemistry. The alkaline in the semen reacts with the acidic pH in your vagina. It’s like turning up the volume on something that was already playing in the background. The presence of Bacterial Vaginosis bacteria just adds to the volume.
3. If it’s an STD, do I necessarily have to have other symptoms?
Nope. STDs are silent killers. Chlamydia and Gonorrhea have no smell at all. Trichomoniasis has a smell with discharge, but not necessarily a strong one. The only way to know for sure what’s wrong with your body is to get tested.
4. Can I differentiate between Bacterial Vaginosis and trichomoniasis just by smell?
Honestly? No. The internet claims that yes, you can. But no. Both have a bad smell. The only difference is the discharge. But discharge comes in different colors. The only way to know for sure what’s wrong with your body is to get tested.
5. Why does this keep happening with the same partner?
This one hits me on an emotional level. The fact that there’s a recurring smell with one partner does not necessarily mean that partner cheated on you or gave you an STD. The fact is, everyone's body chemistry is different, and it can affect the natural balance of your own body.
6. Will showering more often solve the problem?
Yes, I know it sounds tempting to think that showering more often will solve the problem and that a good dose of soap will chase away the smell and the symptoms. The problem with this line of thinking is that it can, in fact, exacerbate the problem and make BV worse.
7. How long do I have to wait before I go get tested?
It's worth noting that while it's best to get tested for bacterial STDs like Chlamydia and Gonorrhea 7-14 days after being exposed to them, it's also worth noting that this does not apply to BV.
8. Will BV go away on its own?
Yes and no. The fact is, sometimes it will go away on its own, and sometimes it won't. If you're finding that you're going in and out of a cycle where it goes away and then comes right back after you have sex, then it's probably a good idea to stop white-knuckling it and go get tested.
9. Does a fishy smell mean I’m a dirty, disgusting person?
No! I think it's worth noting that this question comes up a lot, and I think it's worth saying that a fishy smell does not, in fact, say anything at all about a woman's level of cleanliness or worth.
10. What's the smartest next step I can take if I’m still unsure?
Data over panic. If the smell lingers or you are still uncertain, there is a discreet test you can use so that you are dealing with facts rather than fears. Then, once you know what is going on, you can deal with it calmly and move on with your life, and that is the whole point.
Before You Spiral: A Calm Decision Framework
If you’re standing in your bathroom right now wondering what to do next, here’s the grounded approach:
- If the smell is new and fades within a day → monitor.
- If it lingers 2–3 days → consider BV testing.
- If it comes with irritation, colored discharge, or recent high-risk exposure → test for STIs.
If you want fast clarity without waiting weeks for appointments, discreet panels are available through STD Test Kits. Multi-infection panels like the 6‑in‑1 At‑Home STD Test Kit allow screening for common infections in one step.
Clarity reduces anxiety. Guessing feeds it.
How We Sourced This Article: This guide was developed using current clinical guidance from leading medical authorities, peer-reviewed research on the vaginal microbiome and bacterial vaginosis recurrence, and lived-experience reporting to reflect real-world concerns. Approximately fifteen sources informed the full analysis. Below are six of the most authoritative and accessible references. All external links were verified at time of publication and open in a new tab for reader transparency.
Sources
1. Mayo Clinic – Bacterial Vaginosis Overview
3. WHO – Sexually Transmitted Infections Fact Sheet
4. About Bacterial Vaginosis (BV) (CDC)
5. Vaginitis - Symptoms & causes (Mayo Clinic)
About the Author
Dr. F. David, MD, is a board-certified infectious disease specialist with a special interest in the prevention, diagnosis, and treatment of STIs. He has a unique ability to provide precise medical information with a stigma-free, sex-positive attitude.
Reviewed by: A. Morgan, NP-C | Last medically reviewed: February 2026
This article is for informational purposes and does not replace medical advice.