Quick Answer: Anal itching after sex is usually caused by friction, minor irritation, hemorrhoids, or yeast, but it can also signal rectal STDs like gonorrhea, chlamydia, herpes, or syphilis. If itching lasts more than a few days, worsens, or follows unprotected anal sex, testing is recommended.
“I Thought It Was Just Lube Burn”
Marcus, 27, had receptive anal sex with a new partner. They used a condom, but not much lube. The next day he noticed itching. No discharge. No pain. Just a nagging irritation that wouldn’t quit.
“I kept telling myself it was just friction. But by day four, I couldn’t stop thinking about it. I felt embarrassed even considering an STD test. Like I was being dramatic.”
Marcus eventually got a rectal swab test. It came back positive for rectal chlamydia. He had zero other symptoms. No discharge. No bleeding. No fever. Just itching.
This is the part no one tells you loudly enough: rectal STDs are often subtle. According to the CDC, rectal gonorrhea and chlamydia infections are frequently asymptomatic, especially in men who have sex with men, but they can still cause mild irritation, itching, or discomfort. Left untreated, they can persist silently.
Testing isn’t dramatic. It’s data. And data ends spirals.

People are also reading: Swollen Lymph Nodes in Groin: STD or Something Else?
Let’s Start With the Obvious: Friction and Irritation
Anal tissue is delicate. It wasn’t designed for friction the way other parts of the body are. Even with a condom, even with consent, even with experience, micro-tears and surface irritation can happen. Especially if there wasn’t enough lubrication.
Post-sex irritation typically shows up within 24 hours. It may feel like mild itching, slight swelling, or tenderness. The good news? It usually improves within 2–3 days. No discharge. No worsening pain. No spreading rash.
If the itching is fading instead of escalating, that’s your first clue it’s likely mechanical irritation, not infection.
Hemorrhoids: The Overlooked Culprit
Sex can increase pressure in the rectal veins. If you already had small hemorrhoids (many adults do and don’t know it), intercourse can irritate them. Hemorrhoid itching tends to feel localized and persistent, often worse after bowel movements.
You might notice a small lump, mild bleeding on toilet paper, or a heavy sensation. What you typically won’t see with hemorrhoids is discharge, fever, or systemic symptoms.
Hemorrhoids don’t mean you did anything wrong. They mean you’re human.
Yeast, Sweat, and the Microbiome Shift
Anal sex can change the local moisture and bacterial balance. Add tight underwear, sweat, or leftover lubricant, and yeast can flourish. Anal yeast infections cause itching that can feel intense and sometimes slightly raw.
Unlike many bacterial STDs, yeast itching often feels constant and may come with redness or a shiny rash. It doesn’t usually cause rectal discharge or deep internal pain.
If antifungal cream improves symptoms within a few days, yeast was likely the issue. If nothing changes, it’s time to widen the investigation.
When It’s Not Just Irritation: STD Causes of Anal Itching
This is where we shift from guesswork to medicine. Several sexually transmitted infections can infect the rectum, even without vaginal symptoms, even without ejaculation, even without obvious sores.
Rectal infections are diagnosed with swabs or blood tests. Urine tests alone often miss them. That’s an important distinction most people don’t learn until after a false negative.
Here’s how the most common rectal STDs show up.
Rectal Gonorrhea and Chlamydia
Both gonorrhea and chlamydia can infect rectal tissue through receptive anal sex. According to the CDC’s STI Treatment Guidelines, rectal infections are frequently asymptomatic, but when symptoms do occur, they may include:
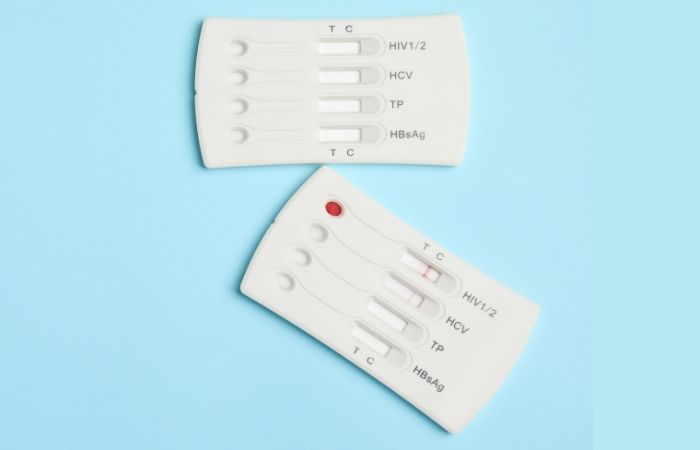
Figure 1. Symptom comparison of rectal gonorrhea and chlamydia. Many infections cause minimal or no symptoms.
If your itching began 3–10 days after unprotected anal sex and isn’t improving, a rectal swab test is the most accurate way to rule these out.
And here’s the empowering part: both are treatable with antibiotics. Early testing protects you and your partners.
Here’s what makes rectal STDs tricky: up to 70–85% of rectal chlamydia infections may be asymptomatic in some populations. Rectal gonorrhea is also frequently silent.
That means itching might be the only sign, or there may be no sign at all.
This is why routine screening is recommended for sexually active individuals who have receptive anal sex, especially men who have sex with men. It isn’t about labeling behavior. It’s about matching testing to anatomy.
Anal Herpes: Itching Before the Sores
Herpes (HSV-1 or HSV-2) often starts with tingling, itching, or burning before visible blisters appear. This prodrome phase can last hours to days.
The itching tends to feel more electric or nerve-like. You may feel tenderness when sitting. Within a few days, small clustered blisters or ulcers may appear around the anus.
Not everyone sees obvious sores. Some outbreaks stay internal. According to research published in the journal Sexually Transmitted Diseases, subclinical herpes shedding is common, even when visible lesions are absent.
If itching is followed by pain, blistering, or flu-like symptoms, herpes testing (swab if lesions are present, blood test if not) becomes important.
Syphilis and HPV: The Less Common but Real Causes
Syphilis can cause painless sores (chancres) that may go unnoticed if they’re internal. Secondary syphilis may cause rash, including around the anal area. Itching isn’t always prominent, but irritation can occur.
HPV can lead to anal warts, which may itch or feel raised. These develop weeks to months after exposure, not overnight.
Both infections require medical evaluation. Both are manageable when caught early.
When to Test After Anal Itching
This is where panic turns into plan.
If itching started within 24 hours and is already improving, you can monitor. If it persists beyond 3–5 days, worsens, or follows condomless anal sex, testing becomes reasonable and proactive.
Testing windows matter. Here’s a simplified timing guide.
Figure 2. Approximate testing windows for common rectal STDs. Always consult current CDC guidelines for precise recommendations.
If you test too early, you risk a false negative. If you test within the optimal window, you get clarity. And clarity is powerful.
Rectal Swab vs Urine Test: Why It Matters
This is one of the most common mistakes people make: they get a urine test and assume it checked everything. It didn’t.
Urine testing detects infections in the urethra. Rectal infections live in rectal tissue. If you had receptive anal sex, you need a rectal swab to properly test for gonorrhea and chlamydia.
According to CDC STI guidelines, extragenital testing significantly increases detection rates in people who engage in anal sex. Translation? You can test negative in urine and still have a rectal infection.
This isn’t about fear. It’s about accuracy.
People are also reading: Pelvic Pain: STD, Ovarian Cyst, or Something Else?
When It’s Probably NOT an STD
Let’s reduce anxiety with clinical logic.
If your itching:
- Started immediately after sex
- Is improving each day
- Has no discharge, sores, or systemic symptoms
- Resolved within 3 days
- It’s more likely friction or irritation.
If it:
- Started several days later
- Is persistent or worsening
- Includes discharge, bleeding, sores, or pain
- Occurred after condomless anal sex
- Testing is reasonable.
Not because you did something reckless. Because you deserve to know.
What About Nighttime Itching?
Night itching can intensify simply because your brain has fewer distractions. You feel everything more. That doesn’t automatically mean infection.
However, severe itching at night can also be associated with pinworms, yeast, or inflammatory skin conditions. STDs are not the most common cause of isolated nighttime itching, but if exposure risk exists, they remain part of the differential.
This is why symptom context matters more than a single sensation.
Testing From Home: Private, Fast, and Accurate
If your anxiety is building, waiting weeks for a clinic appointment can make it worse. That’s where discreet at-home testing becomes empowering instead of frightening.
You can explore options directly at STD Test Kits. Their collection includes targeted and combination panels designed for privacy and speed.
For broader screening, especially after a hookup where you’re unsure what you were exposed to, a Combo STD Home Test Kit can screen for multiple infections at once. It’s discreet, fast, and removes the waiting-room anxiety.
Testing is not an admission of guilt. It’s self-respect.
If It Is Positive: What Happens Next?
Most bacterial rectal STDs are treated with antibiotics. Herpes is managed with antiviral medication. Syphilis is treated effectively with penicillin. These are medical conditions, not moral verdicts.
Partners can be notified calmly and compassionately. Many public health departments even offer anonymous partner notification tools.
The sooner you test, the sooner you move from uncertainty to action.
Why Shame Makes Symptoms Worse
Here’s something the data doesn’t measure well: the psychological spiral.
Shame amplifies physical sensations. Anxiety heightens itch perception. The more you fear what it “means,” the more your nervous system tunes into every sensation.
Anal sex is common. Queer sex is valid. Curiosity is human. Mistakes happen. Protection isn’t perfect. None of that makes you reckless or dirty.
Testing is neutral. Science is neutral. Your worth isn’t up for debate.
How to Decide Tonight
Ask yourself three questions:
- Was there condomless receptive anal sex?
- Has the itching lasted more than 3–5 days?
- Are there additional symptoms like discharge, sores, or pain?
- If the answer to any is yes, testing is reasonable.
If the answer to all is no and symptoms are fading, monitor for a few days. You don’t need to panic. But you also don’t need to guess.
When It’s Just Irritation, And When It’s Something More
Let’s slow this down and get clinical for a minute, not cold, not alarmist. Just observant.
Not all itching means the same thing. Friction from sex tends to feel shallow and surface-level. It shows up quickly, usually within hours, and feels like chafing. It improves steadily over a couple of days. The body heals. End of story.
But infections behave differently. They don’t always arrive immediately. They settle in. The sensation can feel deeper, slightly internal, sometimes paired with a subtle pressure, mucus, or discomfort during bowel movements. And here’s the part that surprises people: many rectal STDs don’t cause obvious discharge at all.
People expect drama. They expect something visible. But rectal gonorrhea and chlamydia are frequently quiet. Herpes can start as tingling or nerve-like itching before any sore appears. The absence of discharge doesn’t rule anything out.
Instead of guessing, clinicians look at patterns, timing, progression, exposure risk, and accompanying symptoms. Here’s how that logic plays out:
Figure 3. Clinical pattern comparison for post-sex anal itching.
Notice what’s missing from that infection column? “Massive obvious discharge.” That’s because it’s not required for diagnosis. Many rectal infections are subtle. Some are completely asymptomatic. The body doesn’t always announce what’s happening inside it.
If itching started immediately and is fading, irritation is likely. If it showed up days later, feels different from simple chafing, or isn’t improving, that’s when testing becomes less about fear and more about clarity.
You’re not trying to label yourself. You’re trying to understand a pattern. And patterns are testable.
How Long Does STD-Related Itching Last?
Here’s the honest answer: untreated bacterial infections like rectal chlamydia or gonorrhea can persist for weeks or months. They don’t just “burn out” in a few days.
Herpes outbreaks typically evolve over 7–14 days, starting with itching or tingling, progressing to lesions, and then healing. Syphilis sores may last 3–6 weeks if untreated.
If itching fades completely within a few days, infection becomes less likely. If it lingers beyond a week or evolves, testing becomes increasingly important.
Anal Itching After Protected Sex, Should You Still Worry?
Condoms are effective in preventing the transmission of STDs. They are one of the best protection measures we have. However, they are not foolproof.
Skin-to-skin STDs, like herpes and HPV, can be spread through areas not covered by the condom. Condoms may tear or slip off. There are also problems with lubrication, causing irritation as well.
If the condom was used correctly and the symptoms are mild and improving, the risk is lower. However, the risk may not be zero, and here’s where timing-based testing can bring peace of mind.

People are also reading: What Does Green or Yellow Discharge Mean?
What Doctors Actually Look For
When clinicians evaluate rectal itching after sex, they consider:
Figure 4. Clinical reasoning framework for rectal itching after sex.
Medicine is rarely about one symptom. It’s about patterns over time.
The Role of Routine Screening
If you have receptive anal sex regularly, routine screening every 3–6 months may be recommended depending on your risk profile. This isn’t about suspicion, it’s preventive care.
Many public health organizations, including the CDC, recommend extragenital screening (rectal and throat testing) for sexually active men who have sex with men and others at risk. Without rectal swabs, infections are missed.
Routine testing removes the drama. It becomes maintenance, like dental cleanings or annual physicals.
When Symptoms Persist But Tests Are Negative
This happens more often than people expect. You test within the right window. Results are negative. But itching continues.
At that point, clinicians consider dermatologic causes like eczema, psoriasis, contact dermatitis, or chronic hemorrhoids. Anxiety itself can also amplify perception of itch long after tissue has healed.
If symptoms persist beyond two weeks with negative testing, a primary care or dermatology evaluation is appropriate. Not because something catastrophic is hiding, but because comfort matters.
Decision Path: What To Do Right Now
If you’re reading this and actively itching, here’s a grounded plan:
- If symptoms started less than 48 hours ago and are improving, monitor.
- If symptoms are stable or worsening at day 3–5, schedule testing.
- If sores, discharge, or bleeding appear, test promptly.
- If anxiety alone is overwhelming you, testing sooner can still be reasonable, even if you may need a repeat test for accuracy.
Waiting strategically is about accuracy. Testing strategically is about empowerment.
FAQs
1. Can anal itching really be the only sign of an STD?
Yes. And that’s the part that messes with people’s heads. We expect drama, pain, discharge, something obvious. But rectal chlamydia or gonorrhea can be subtle. Just a little itching. Maybe a vague discomfort you can’t quite name. If there was exposure, itching alone is enough to justify testing. Quiet infections are still infections.
2. It started the next morning. Isn’t that too fast to be an STD?
Usually, yes. Most bacterial STDs take a few days to show symptoms, if they show any at all. If itching began within 24 hours, friction or irritation is more likely. But here’s the key: watch the pattern. If it fades quickly, that supports irritation. If it lingers or evolves, that’s when we investigate.
3. There’s no discharge. Doesn’t that mean I’m fine?
I wish it were that simple. Many rectal infections cause no visible discharge. People often assume “no goo, no problem,” but that’s not how these infections behave. The rectum doesn’t always advertise what’s happening inside it. Testing is the only way to know for sure.
4. What does herpes itching actually feel like?
People describe it as electric. Tingly. Almost like a nerve waking up under the skin. It’s different from surface chafing. With herpes, itching or burning often comes before blisters appear. Sometimes those blisters are tiny or internal and easy to miss. If the itch feels sharp, localized, and nerve-like, especially followed by soreness, get checked.
5. We used a condom. Should I still be worried?
Condoms dramatically reduce risk, and that matters. But they don’t cover every inch of skin. Herpes and HPV spread through skin contact, not just fluids. That said, if protection was used correctly and symptoms are mild and fading, the odds lean toward irritation. Testing isn’t about panic, it’s about peace of mind.
6. How long should I wait before getting tested?
For rectal gonorrhea and chlamydia, about 7 days after exposure is the earliest reasonable window, with peak accuracy around 14 days. Testing at day two will likely tell you nothing useful. Waiting strategically is frustrating, but it improves accuracy. If anxiety is overwhelming, you can test early, just plan a follow-up test if needed.
7. Can anxiety make itching feel worse?
Absolutely. When you’re hyper-focused on a body part, your brain amplifies sensation. The more you Google, the more you notice every micro-twitch. That doesn’t mean symptoms are imaginary. It means your nervous system is turned up. Testing often quiets that noise because uncertainty is the real amplifier.
8. If I test positive, does that mean I was reckless?
No. It means you’re human. STDs are common. People in long-term relationships get them. People who use condoms get them. People who had one hookup ever get them. Most are treatable. None are moral verdicts. The responsible move is testing and treatment, not self-punishment.
9. What if everything is negative but the itching won’t stop?
Then we pivot. Dermatologic causes like eczema, contact dermatitis, chronic hemorrhoids, or yeast are far more common than people realize. Sometimes the answer isn’t sexual, it’s skin. If symptoms persist beyond two weeks with negative STD tests, a primary care or dermatology visit makes sense. Comfort matters.
10. Is routine rectal testing really necessary if I feel fine?
If you have receptive anal sex, yes, routine screening can be part of standard sexual healthcare. Many rectal infections cause no symptoms at all. Think of it like dental cleanings. You don’t wait for pain to brush your teeth. Preventive testing keeps things simple and drama-free.
You Deserve Answers, Not Assumptions
Anal itching after sex can mean many things. Often, it’s simple irritation that fades on its own. Sometimes it’s hemorrhoids or yeast. And occasionally, it’s a rectal STD that needs treatment.
The difference between panic and power is information. Testing isn’t shameful, it’s strategic. If you’re unsure, don’t wait and spiral. Explore discreet options at STD Test Kits, or consider a broader screen with a Combo STD Home Test Kit. Your results are private. Your health is yours.
Peace of mind is one test away.
How We Sourced This Article: This guide integrates current CDC STI Treatment Guidelines, peer-reviewed research from journals such as Sexually Transmitted Diseases, and clinical consensus statements from Mayo Clinic and NHS resources. Approximately fifteen sources informed this article, including epidemiologic surveillance data on asymptomatic rectal infections. We selected six of the most reader-accessible, authoritative references below. All links were verified to open in a new tab for transparency and accuracy.
Sources
1. CDC Sexually Transmitted Infections Treatment Guidelines
2. Mayo Clinic – Genital Herpes Overview
3. Proctitis, Proctocolitis, and Enteritis - STI Treatment Guidelines (CDC)
4. Anal itching - Symptoms and causes (Mayo Clinic)
5. Sexually Transmitted Proctitis (PMC)
About the Author
Dr. F. David, MD is a board-certified infectious disease specialist focused on STI prevention, diagnosis, and treatment. He combines clinical precision with a direct, stigma-free approach to sexual health education.
Reviewed by: Lauren Mitchell, PA-C | Last medically reviewed: February 2026
This article is for informational purposes and does not replace medical advice.






