Swab vs Blood vs Urine STD Tests: What’s the Real Difference?
Quick Answer: HPV can cause throat and head and neck cancers in men, often with subtle symptoms like a painless lump under the jaw or a persistent sore throat. While there is no routine at-home HPV throat test for men, proactive STD testing, vaccination, and early medical evaluation of symptoms significantly reduce long-term risk.
The BBC article centers on a man who initially noticed what seemed like a harmless lump. He had no idea that HPV, a virus most people associate with cervical cancer, can also cause cancers of the throat, tonsils, and tongue. His experience highlights a critical gap: many men are never told that HPV is one of the leading causes of head and neck cancers today. This blog builds on that story, expanding beyond the headline to explain what HPV does in the body, how symptoms can appear quietly, and how at-home STD testing fits into a larger strategy of awareness, prevention, and control.

People are also reading: Does Gonorrhea Cause Itching? Here’s the Honest Answer
When a Neck Lump Isn’t “Just a Swollen Gland”
A painless lump in the neck is one of those symptoms people Google in private. “Unexplained neck lump.” “Swollen lymph node on one side.” “Lump under jaw that doesn’t hurt.” The search history usually begins with hope, maybe it’s a cold, maybe allergies, and slowly slides toward fear. Mouth cancer symptoms. Head and neck cancer signs. Why won’t this go away?
HPV-related throat cancers often begin in the tonsils or base of the tongue. The first noticeable sign may not be throat pain at all. It can be a swollen lymph node under the jaw because the body is reacting to cancer cells that have already spread locally. That’s why the BBC story matters. It disrupts the myth that cancer always announces itself loudly.
According to the Centers for Disease Control and Prevention (CDC), HPV causes about 70% of oropharyngeal cancers in the United States, and these cancers are significantly more common in men than women. What makes this more complicated is that most HPV infections cause no symptoms at all. The virus can live in the body for years before any visible problem appears.
HPV in Men: The Awareness Gap No One Talks About
For decades, public messaging framed HPV primarily as a women’s health issue. Cervical cancer screening campaigns dominated the conversation. Pap smears became standard. But boys and men often grew up without the same urgency around vaccination or awareness. The BBC article reflects this reality: the patient said he never imagined HPV could affect him this way.
Here’s the truth. HPV is incredibly common. The CDC estimates that nearly all sexually active people will contract at least one strain of HPV at some point in their lives. In most cases, the immune system clears it naturally within two years. But certain high-risk strains, particularly HPV-16, are strongly linked to throat cancer.
There is currently no approved routine HPV throat screening test for men. That’s where confusion sets in. People search “Is there an HPV test for men?” or “How do you test for oral HPV?” and find mixed answers. While cervical HPV screening exists, oral HPV testing is not standardized for asymptomatic individuals. That doesn’t mean prevention is impossible, it means awareness and broader sexual health monitoring become even more important.
Symptoms People Ignore, Until They Don’t
The danger with HPV-related throat cancer is not dramatic pain. It’s subtle persistence. A sore throat that doesn’t go away. Difficulty swallowing that feels minor at first. Ear pain when swallowing without signs of infection. A single swollen lymph node that remains for weeks.
These symptoms overlap with common illnesses, which makes self-diagnosis tricky. That’s why duration matters. A viral sore throat improves within days. A bacterial infection responds to antibiotics. But when something lingers beyond two to three weeks, especially without fever or cold symptoms, it deserves evaluation.
The BBC case reinforces a core lesson: early detection changes outcomes. HPV-related throat cancers often respond well to treatment when caught early. But waiting because something “doesn’t hurt” can delay diagnosis.
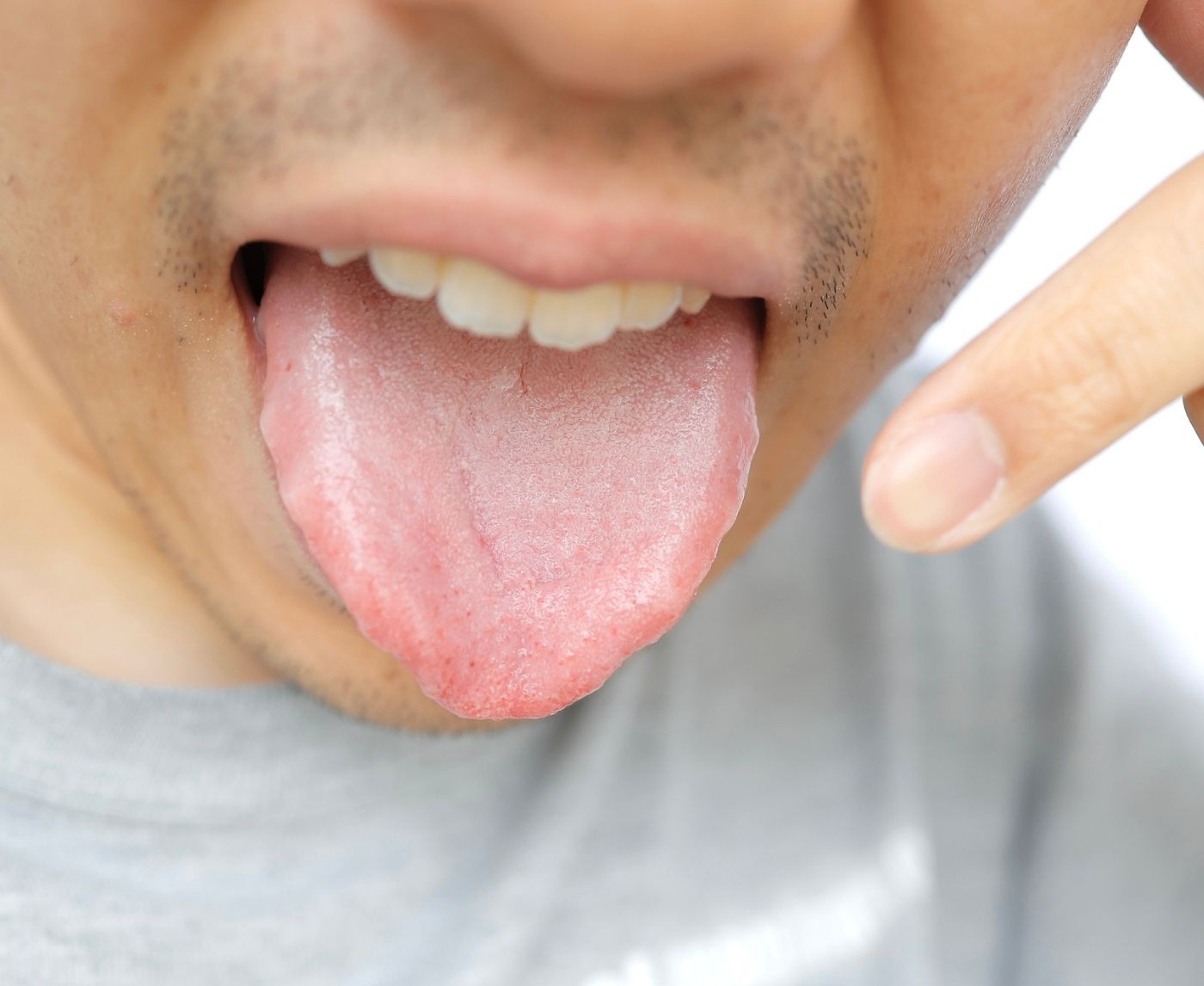
Figure 1. Early warning signs that overlap with common conditions but require evaluation if persistent.
So Where Does At-Home STD Testing Fit Into This?
This is the part many people misunderstand. There is no FDA-approved at-home screening test specifically for detecting HPV in the throat in asymptomatic men. However, that does not make at-home testing irrelevant. In fact, it becomes part of a bigger prevention strategy.
Most high-risk HPV infections are transmitted through intimate skin-to-skin contact, including oral sex. Regular comprehensive STD testing reduces the likelihood of undiagnosed infections overall and encourages ongoing engagement with sexual health care. When people test consistently for infections like chlamydia, gonorrhea, syphilis, and HIV, they are more likely to notice changes in their bodies and seek care earlier.
If you are sexually active and unsure of your current status, starting with a discreet at-home panel from STD Test Kits gives you clarity about common infections. While it won’t diagnose throat cancer, it places you in a proactive posture, and that mindset matters.
For example, a combo STD home test kit allows you to screen for multiple infections in one private step. Peace of mind about what you don’t have is powerful. It clears mental space so you can focus on persistent symptoms that need medical evaluation.
Understanding Risk Without Panic
The phrase “throat cancer from oral sex” tends to spark anxiety. But context is essential. HPV is common. Most infections never become cancer. The body’s immune system clears the virus in the majority of cases. What increases risk is persistent infection with high-risk strains over many years.
Vaccination dramatically reduces this risk. The HPV vaccine protects against the strains most commonly associated with cancer. Public health organizations now recommend vaccination for both boys and girls, ideally before sexual debut, but catch-up vaccination is available for many adults as well.
The BBC story is not meant to scare people away from intimacy. It is meant to close an awareness gap. Knowing that HPV can affect men’s throat health allows earlier medical attention when symptoms arise. That is empowerment, not fear.
How Oral HPV Spreads, And Why It Can Stay Invisible for Years
When people hear “HPV,” they often picture genital warts or cervical screening appointments. They don’t picture the back of the throat. They don’t picture tonsils. They definitely don’t picture a cancer diagnosis years after a relationship ended. But oral HPV spreads the same way genital HPV does: through intimate skin-to-skin contact, including oral sex.
The virus doesn’t need visible sores. It doesn’t require ejaculation. It doesn’t announce its arrival. A person can contract HPV from a single encounter and never know it. Most of the time, the immune system clears the infection quietly within one to two years. That’s why HPV is so common and often harmless. But in a small percentage of cases, high-risk strains persist. Persistence, not exposure alone, is what increases the risk of cancer.
According to the CDC, HPV is the most common sexually transmitted infection in the United States, and HPV-16 is the strain most strongly associated with oropharyngeal cancers. These cancers now outnumber cervical cancer cases in some populations, particularly among men. That shift is what makes the BBC story more than just a headline, it reflects a changing epidemiological reality.
Latency, Persistence, and Why Symptoms Can Appear Years Later
One of the most disorienting aspects of HPV-related throat cancer is timing. Someone may ask, “How did this happen? I haven’t had a new partner in years.” The answer lies in viral latency. HPV can remain dormant or undetected in the body for a long time before causing cellular changes.
This delayed timeline fuels stigma. People assume recent behavior must be the cause. In reality, the virus could have been present for years. That’s why blame is medically misplaced. HPV infection is common. Cancer development is rare. But when persistent high-risk strains cause abnormal cell growth, symptoms may not surface until much later.
Understanding the difference between infection, persistence, and cancer development helps reduce panic while reinforcing vigilance.
Figure 2. Simplified progression timeline from HPV exposure to possible cancer development.
Why There Isn’t a Routine HPV Throat Test for Men
This is one of the most frustrating realities for anxious readers. People search “at home HPV test for men” or “oral HPV screening kit” hoping for a simple answer. Unlike cervical screening, there is no standardized, FDA-approved routine screening test for oral HPV in asymptomatic men.
Why? Because HPV infections in the mouth are often transient. Testing positive for oral HPV does not necessarily predict cancer. The medical community has not yet established a screening threshold that reliably identifies who will develop disease versus who will clear the virus naturally. Screening programs must balance benefit against unnecessary alarm.
Instead, early detection relies on symptom awareness and clinical evaluation. Persistent lumps, unexplained swallowing changes, or chronic sore throat deserve assessment by a healthcare professional. Imaging and biopsy, not viral swabs, are how throat cancers are diagnosed.

People are also reading: Herpes or HPV from Oral Sex? Here’s What Actually Happens
At-Home Testing as Part of a Bigger Sexual Health Strategy
Even though you cannot swab your throat at home for definitive HPV cancer screening, regular STD testing still plays a protective role. Why? Because proactive sexual health behavior builds awareness patterns. People who test consistently are more likely to recognize abnormal symptoms early instead of dismissing them.
At-home testing also removes barriers. Privacy concerns, stigma, scheduling conflicts, and geographic isolation often delay clinic visits. A discreet kit ordered online allows people to stay engaged with their health without added stress. That engagement creates familiarity with one’s body and health status.
Using a comprehensive option like a combo STD home test kit ensures screening for infections that can cause long-term complications if untreated. While HPV-related throat cancer requires medical evaluation for persistent symptoms, maintaining overall STD awareness reduces overlapping risks and keeps prevention conversations active.
Risk Factors That Increase HPV-Related Throat Cancer Odds
Not everyone exposed to HPV develops cancer. Risk increases when certain factors overlap. Persistent infection with high-risk strains is central, but immune suppression, tobacco use, and heavy alcohol consumption can amplify the likelihood of malignant changes.
Men are statistically more likely than women to develop HPV-related throat cancers. Researchers are still studying why, but differences in immune response and viral persistence appear to play a role. The key takeaway is not fear, it’s understanding that awareness gaps disproportionately affect men.
Vaccination remains one of the most effective prevention tools available. The HPV vaccine protects against high-risk strains responsible for most HPV-related cancers. If you or your partner are eligible and unvaccinated, discussing vaccination with a healthcare provider is a powerful protective step.
What Early Detection Actually Looks Like
Early detection is not a dramatic emergency room visit. It often begins with something simple: a primary care appointment after a symptom lingers. A clinician may examine the throat, order imaging, or refer to an ear, nose, and throat specialist. If something suspicious appears, a biopsy confirms diagnosis.
The BBC story demonstrates that catching cancer before it spreads extensively can preserve function and improve survival. HPV-related throat cancers, when treated early, often respond well to therapy. That’s why persistence is the red flag, not intensity.
If you are monitoring symptoms while maintaining routine STD screening through STD Test Kits, you are already operating from a position of proactive control. Testing doesn’t replace medical evaluation for concerning symptoms, but it complements a broader commitment to health literacy and early action.
Rapid Tests, Lab Tests, and the Anxiety in Between
When someone reads a headline about HPV and throat cancer, the instinct is immediate: “I need to get tested.” That urgency is understandable. But clarity requires precision. There is a difference between testing for common sexually transmitted infections and diagnosing HPV-related throat cancer. Understanding that difference prevents both false reassurance and unnecessary panic.
Rapid at-home STD tests are designed to detect infections such as HIV, syphilis, chlamydia, and gonorrhea. These infections have defined window periods and established screening guidelines. HPV-related throat cancer, on the other hand, is diagnosed through physical examination, imaging, and biopsy, not a home viral swab.
This distinction matters because some people confuse a negative STD panel with a clean bill of health for every possible infection. A comprehensive panel from STD Test Kits provides important insight into your sexual health status, but persistent throat symptoms still require medical evaluation. Testing is powerful. It just needs to be used appropriately.
Figure 3. Different testing pathways serve different purposes. Screening is not the same as cancer diagnosis.
When to Test After Sexual Exposure, And When to Wait
Another common reaction to HPV-related headlines is retrospective anxiety. “That hookup six months ago.” “That partner from years back.” Timing questions begin stacking up. It’s important to separate two different timelines: standard STD window periods and long-term HPV persistence.
For infections like chlamydia and gonorrhea, testing is most accurate about 7 to 14 days after exposure. HIV antigen/antibody tests detect infection as early as 18 to 45 days after exposure, depending on the test type. Syphilis blood tests may take 3 to 6 weeks to turn positive. These infections have measurable detection windows.
HPV does not follow the same immediate testing rhythm. Most infections clear naturally within two years. There is no recommended routine oral HPV screening after a single exposure because detection alone does not predict cancer development. What matters more is monitoring for persistent symptoms and maintaining vaccination status when eligible.
If your anxiety is rooted in a recent encounter, beginning with a comprehensive screening panel can provide reassurance about common infections. A combo STD home test kit allows you to address multiple concerns at once, reducing the mental spiral that often accompanies waiting.
Living in the Waiting Period: The Emotional Side of Symptom Uncertainty
There’s a particular kind of silence that follows a symptom. You notice a lump. You swallow again to check if it hurts. You press your fingers under your jaw in the mirror. The mind races ahead of the body.
Many people delay medical visits because they fear confirmation more than uncertainty. The BBC story illustrates how easy it is to minimize something that doesn’t feel urgent. But waiting is not the same as ignoring. Waiting responsibly means tracking duration. Two days is one thing. Three weeks without improvement is another.
Engaging in regular STD testing helps create a rhythm of health maintenance. That rhythm builds confidence. Instead of panicking at every bodily change, you begin distinguishing between routine fluctuations and symptoms that persist beyond reason. Knowledge reduces noise.
Retesting, Reinfection, and Staying Ahead of Risk
For bacterial STDs, retesting is often recommended about three months after treatment to rule out reinfection. Reinfection is common not because treatment fails, but because partners may not have been treated simultaneously. HPV operates differently. There is no antibiotic course that eliminates it instantly. Clearance depends on immune response.
If you are vaccinated, your risk of high-risk HPV strains is significantly reduced. If you are unvaccinated and eligible, vaccination remains protective even after sexual debut. Prevention is layered. Vaccination, routine STD screening, symptom awareness, and early clinical evaluation all work together.
Retesting for other STDs ensures you are not managing overlapping infections that could complicate overall health. Maintaining routine screening through a trusted provider or discreet home service keeps you in a forward-moving position rather than a reactive one.
Privacy, Discretion, and Why Many People Choose At-Home Testing
One reason the BBC story resonates is that it involves something deeply personal. Sexual health often feels private, even isolating. Many individuals avoid clinics because of embarrassment, scheduling constraints, or lack of access. At-home testing changes that dynamic.
Discreet shipping, private results, and the ability to test on your own schedule reduce friction. When friction decreases, testing frequency increases. Increased testing leads to earlier detection of treatable infections. While HPV-related throat cancer requires clinical evaluation for suspicious symptoms, the habit of private proactive screening fosters earlier action overall.
Your results are your information. Your decisions remain yours. Privacy empowers responsibility instead of delaying it.
If a Result Is Positive, What Happens Next?
A positive STD result does not equal catastrophe. It equals clarity. Most bacterial STDs are treatable with antibiotics. Viral infections like HIV are highly manageable with modern therapy. Early detection protects long-term health and partners.
If you ever receive a positive result from a home kit, confirmatory testing with a healthcare provider may be recommended depending on the infection. Treatment pathways are well established and often straightforward. The same principle applies to suspicious throat symptoms: confirmation comes from professionals, and earlier is better.
The BBC patient’s experience underscores this truth. Early intervention preserved his ability to speak and function. Acting quickly does not mean assuming the worst. It means respecting your body’s signals.

People are also reading: Thick White Discharge With No Smell: What It Really Means
FAQs
1. Can HPV really cause throat cancer in men?
Yes, and that’s the part many men were never told. For years, HPV messaging centered on cervical cancer, so a lot of guys grew up thinking it “wasn’t their issue.” But high-risk strains like HPV-16 are now responsible for most HPV-related throat cancers, and these cases are more common in men than women. The virus itself is common. Cancer is not. But awareness shifts outcomes.
2. I have a lump under my jaw. Should I panic?
No. Panic rarely helps anything. Most neck lumps are swollen lymph nodes reacting to infection, a cold, dental irritation, even allergies. What matters is time. If that lump sticks around longer than two or three weeks, grows, or doesn’t come with typical cold symptoms, that’s when you book the appointment. Calm action beats spiraling every time.
3. Why isn’t there a routine HPV throat test for men?
Because testing positive for oral HPV doesn’t tell doctors what will actually happen next. Many oral HPV infections clear naturally within a year or two. A test that simply says “HPV detected” would cause fear without clearly predicting cancer risk. Medicine avoids screening tools that create more anxiety than benefit. Instead, doctors focus on persistent symptoms and structural changes.
4. If my STD panel is negative, am I in the clear?
You’re in the clear for what that panel tested. That’s important. But standard panels don’t routinely screen for oral HPV in men. Think of STD screening as one layer of protection. It’s powerful, but it’s not an x-ray of your throat. Persistent symptoms still deserve real-world evaluation.
5. How common is oral HPV, really?
More common than most people realize. The majority of sexually active adults will be exposed to HPV at some point. Most will never know it happened. Most will clear it naturally. The difference between “common infection” and “rare cancer” is persistence over years, not a single encounter.
6. Does this mean oral sex is dangerous?
It means oral sex, like any intimate contact, carries some risk. Risk is part of being human. But risk is not destiny. Vaccination dramatically lowers the chance of high-risk strains. Most exposures do not lead to cancer. Sexual health is about informed decisions, not fear-based avoidance.
7. How long would it take for HPV to turn into cancer?
Typically many years, often five to fifteen or more. This isn’t something that develops weeks after exposure. That long timeline is why blame doesn’t belong in the conversation. The virus can linger silently for years before causing trouble, if it causes trouble at all.
8. I have a sore throat that won’t go away. What’s the line between normal and concerning?
A sore throat from a cold improves. A sore throat from allergies fluctuates. A sore throat that quietly lingers for three weeks without obvious cause? That deserves attention. Especially if it’s paired with difficulty swallowing, a one-sided neck lump, or unexplained ear pain. Duration changes the story.
9. Is the HPV vaccine still worth it if I’m already sexually active?
Often, yes. The vaccine protects against multiple high-risk strains. Even if you’ve been exposed to one strain, you may not have encountered others. Vaccination is prevention moving forward. It doesn’t rewrite the past, it protects the future.
10. What’s the most grounded step I can take today?
Start with information, not imagination. If you’re eligible, talk to a provider about vaccination. Keep up routine STD screening so you’re not carrying untreated infections that cloud the picture. And if something in your body feels “off” for longer than it should, trust that instinct enough to get it checked. Action is steadier than fear.
You Deserve Awareness, Not Fear
The BBC story is not a warning to panic. It is a reminder that subtle symptoms matter and that HPV is not only a women’s health issue. A painless lump under the jaw is easy to dismiss. A sore throat that lingers is easy to explain away. But awareness shifts the timeline. Awareness shortens delay.
Taking control of your sexual health does not require alarm. It requires consistency. Begin with routine screening through STD Test Kits, consider vaccination if you are eligible, and seek medical evaluation when symptoms persist. If you want comprehensive screening in one step, a combo STD home test kit provides discreet clarity. Your health decisions are not confessions. They are acts of self-respect.
How We Sourced This Article: We reviewed current epidemiological data from the Centers for Disease Control and Prevention, National Cancer Institute resources, peer-reviewed oncology research, and public health vaccination guidelines. We also analyzed reporting from BBC News to contextualize lived experience with medical evidence. In total, approximately fifteen sources informed this piece. Below are six authoritative references selected for clarity and public accessibility.
Sources
1. World Health Organization – Human Papillomavirus (HPV)
2. BBC News – HPV Risk Appeal from Father Who Nearly Lost His Tongue
3. HPV and Oropharyngeal Cancer | CDC
4. Basic Information about HPV and Cancer | CDC
5. HPV and Cancer | National Cancer Institute
About the Author
Dr. F. David, MD is a board-certified infectious disease specialist focused on STI prevention, diagnosis, and treatment. He blends clinical precision with a sex-positive, stigma-free approach and is committed to expanding access to discreet testing options.
Reviewed by: Jordan Malik, MPH | Last medically reviewed: February 2026
This article is for informational purposes and does not replace medical advice.