Quick Answer: You have every right to ask a donor or surrogate about recent STD/STI testing. It’s not rude, it’s essential. Most clinics require screening, but if you're using a known donor or doing home insemination, you’ll need to take the lead and document it.
Who This Article Is For (And Why You Might Be Hesitating)
If you’re pursuing parenthood through sperm donation, egg donation, surrogacy, or home insemination, this guide is for you, especially if your fertility path feels less “traditional” and more DIY. Maybe you're a queer couple using a known donor. Maybe you’re a solo parent working with a surrogate outside a clinic. Or maybe your fertility plan involves both partners and you're navigating sensitive health disclosures together.
These journeys are deeply personal, often complicated by social dynamics: friends as donors, siblings as carriers, or romantic partners becoming co-parents. That’s where the hesitation creeps in: “Am I being invasive? Will they feel judged? What if they say no?”
We’re here to say this clearly: STD testing is not a moral judgment. It’s medical, relational, and entirely within your rights to request. And yes, you can ask. With clarity. With compassion. And with full legal and emotional backing.
People are also reading: Can You Trust a “Not Detected” STD Result?
What STD Testing Looks Like for Donors and Surrogates
Let’s break down what “testing” really means in this context. Most established sperm banks and fertility clinics follow strict FDA and ASRM (American Society for Reproductive Medicine) guidelines that mandate comprehensive STI screening for both anonymous and directed donors. But if you're working with a known donor, or navigating non-clinic surrogacy, those systems don’t apply automatically.
Here’s what should be included in a full panel for donors and gestational carriers:
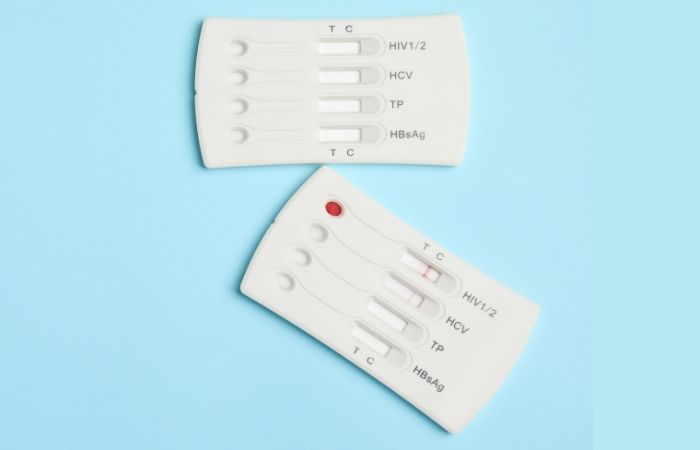
Figure 1. Common STI screening panel for reproductive donors and surrogates
If you're using an at-home or informal pathway (e.g. insemination by syringe), these tests aren’t guaranteed. STD Test Kits offers at-home versions of many of these screens, discreet, fast, and without lab visits.
How to Actually Ask (Without Making It Awkward)
Let’s be real: asking someone to take an STD test can feel like you’re accusing them of something. But reframed correctly, it becomes a shared act of care, not suspicion.
Start with context, not confrontation. “I’ve been reading about the medical requirements before insemination and I’d love us both to be up-to-date on our testing.” That’s very different from: “I need to know if you’re clean.”
Script Example for a Known Donor
“Hey, as we’re getting closer to insemination, can we both do updated STI panels? It’s part of most clinic protocols, and it just feels smart and protective for everyone involved.”
Script Example for a Surrogate Conversation
“Before we finalize our agreement, I want to make sure we’ve both had a chance to review testing timelines. Would you be comfortable sharing your last panel or doing one together?”
When framed as mutual responsibility, not one-sided vetting, these conversations can build trust, not tension. And if someone refuses? That’s useful information, too.
Whether it's a one-time donation or a full surrogacy journey, you deserve transparency before anyone’s body is involved.
Are There Laws About STD Testing for Donors and Surrogates?
Short answer: yes, but they’re uneven. In the U.S., the FDA mandates STI testing for anonymous sperm and egg donors. That includes HIV, hepatitis, syphilis, chlamydia, and gonorrhea. These tests must be performed within 7 days of donation, and samples are often frozen for a quarantine period before use.
But for known donors and gestational surrogates, especially in informal or private arrangements, no federal testing law applies. Instead, it’s often governed by state law, private contracts, and clinic discretion. And even then, some clinics may not require herpes or HPV testing, despite their potential impact.
That means one thing: if you don’t ask, it might not happen.
This legal gray zone puts the burden on intended parents to advocate for thorough screening. Don’t assume that “the clinic is handling it.” Ask what’s included, get the results in writing, and when needed, order supplemental tests yourself.
Not sure what’s missing? You can use this combo STD kit to double-check status for peace of mind, especially if you’re days away from insemination or embryo transfer.
Home Insemination, Queer Families, and the Testing Gap
For queer couples, single parents by choice, or families using donor-conceived pathways outside of traditional clinics, STD testing can fall through the cracks. Some sperm donations happen in private agreements, via syringe insemination at home. Others use frozen samples from small banks without clear documentation.
Jesse, 34, and their partner Sam used a longtime friend as a known sperm donor:
“We all trusted each other, but no one really knew what tests were needed. We googled things like ‘can you get herpes from sperm?’ at 2AM. We ended up using an at-home chlamydia test just to be safe.”
They later found out their donor had never been tested for CMV, a virus that could seriously affect pregnancy outcomes if the surrogate wasn’t immune.
Even loving, well-intentioned arrangements need structure. It’s not about trust, it’s about documentation. Especially when timing matters, and results may influence frozen sample use or medical clearance.
If you’re navigating home insemination, STD testing should be part of your checklist, just like ovulation tracking and consent forms. STD Test Kits offers discreet options that arrive in days, with results in minutes.
Herpes, HPV, and Other “Invisible” Infections
Here’s the tricky truth: many of the infections that most affect fertility and pregnancy, like herpes and HPV, aren’t always included in standard donor panels. Why? Because they’re common, chronic, and not always seen as disqualifying. But that doesn’t mean they don’t matter.
Let’s break that down:
Figure 2. Common infections often overlooked in donor/gestational carrier testing
Requesting herpes or CMV testing may feel awkward, especially when it’s not on the “required” list. But that doesn’t mean it’s overkill. It’s risk reduction. And when framed as a mutual effort to protect everyone, it lands better than you'd think.
What If They Say No?
This is the hardest part, emotionally and logistically. If a donor or surrogate refuses STD testing or gets defensive when asked, it’s a flag. But what it signals isn’t just about medical risk, it’s about communication, power, and trust.
Even if someone agrees to test but doesn’t share the results, or only gives verbal reassurance, you’re left with doubt. That doubt doesn’t just live in your head; it follows you into every fertility appointment, every beta wait, every ultrasound.
You deserve better than maybe. You deserve documented, mutual clarity. And if that means walking away from a donor who won't test? That’s not failure. That’s protection.
Need help navigating the conversation again? Bookmark this: “I care about your comfort and mine, and I want us both to feel protected. Testing helps make that real.”

People are also reading: Is It Time for an STD Test? 6 Signs You Shouldn’t Ignore
What Happens If They Test Positive?
First: don’t panic. Many STDs are treatable, and even incurable ones like herpes or HIV can be managed in the context of fertility plans. The key is transparency, treatment, and updated planning.
If your donor or surrogate tests positive for:
- Chlamydia or gonorrhea: Treatment is fast and often clears within 7–10 days. Retesting is required before continuing.
- HIV: With an undetectable viral load, many people living with HIV can safely donate in specific settings under specialist supervision.
- Herpes: You can adjust timing, avoid outbreaks, and reduce risk with medication or sperm washing if needed.
This is where clinic oversight and expert guidance help. But if you’re navigating this without a clinic, retesting and documentation matter even more.
Whatever the result, a positive test isn’t the end of the road. But hiding results? That’s a roadblock you don’t want to ignore.
Privacy, Shipping, and Discreet Testing Options
Let’s talk about logistics. Because when you're in the middle of coordinating donors, carriers, clinic dates, and legal paperwork, the last thing you want is a package labeled “STD TEST KIT” showing up on your doorstep, or theirs.
That’s why discreet delivery matters. STD Test Kits ships in plain, unbranded packaging with nothing indicating what’s inside. There’s no pharmacy pickup, no awkward face-to-face. Just a quiet box with everything you need to get answers fast.
Shipping timelines are tight, kits usually arrive within 1–3 business days in most U.S. locations, and results for rapid tests are available in under 15 minutes once collected. That means you can go from “we need to talk” to “we’ve both tested and feel good moving forward” in less than a week.
And for those navigating surrogacy across state lines, remote egg donation, or long-distance donor arrangements? These tests ship nationally, so everyone involved can test from where they are.
Why This Conversation Isn’t Just About Disease
At the heart of this is something deeper than infection risk. It’s about consent. About full-body autonomy, for you, your partner, your surrogate, and even your future child. Knowing someone’s STI status isn’t invasive, it’s collaborative care.
Shame has no place in your fertility plan. Neither does secrecy. When we normalize testing as a baseline expectation, not an accusation, we open the door to healthier relationships, smoother contracts, and more joyful paths to parenthood.
Asking for test results isn’t rude. It’s responsible. And it can be kind, too.
So here’s your green light: Have the talk. Share this article. Put testing into your agreement, your text thread, your shared calendar. Because clear conversations make space for deeper trust.
FAQs
1. Is it rude to ask a sperm donor for their STI results?
Not even a little. It's like asking someone to wash their hands before prepping a meal for your baby, basic, respectful, and non-negotiable. You’re not accusing them of anything. You’re protecting your body, your surrogate, your future child. Ask away.
2. What if I already trust my donor or surrogate?
Great! Trust them to follow through. Testing isn’t a sign of distrust, it’s a team sport. Even long-time partners, siblings, and best friends can carry STIs without knowing. One swab or blood draw now can prevent a whole lot of “why didn’t we check?” later.
3. Can herpes or HPV really affect fertility treatments?
Sometimes, yes. Herpes can complicate timing around embryo transfers if outbreaks happen. Certain strains of HPV are linked to cervical changes that might matter in egg donation or surrogacy. Even if they don’t disqualify someone, knowing helps you plan smarter.
4. Do surrogates get tested more than once?
If they’re going through a licensed agency, usually, yes. Before transfer, during pregnancy, sometimes at specific trimesters. But if you're working independently, you'll need to set the schedule yourself. Include it in your contract and confirm with real receipts, not just promises.
5. My known donor said “I’m clean.” Is that enough?
Honestly? No. “Clean” is not a diagnosis. You need dates, labs, and actual test names. Ask for a screenshot or printed results. If it feels weird to ask, blame your clinic, or better yet, blame this article. We’ll take the heat.
6. What if they test positive for something?
Depends on what and when. Chlamydia? Treatable. Herpes? Manageable. HIV? Still possible in certain settings with sperm washing and specialist care. A positive result isn’t always a stop sign, it’s a fork in the road. You can still move forward safely, just differently.
7. How recent should STI testing be before donation or transfer?
Within 30 days is the gold standard. Some clinics stretch that to 90 days, but sooner is safer, especially for things like gonorrhea or chlamydia that can show up fast. If there’s a new partner or recent travel, retest. No harm in double-checking.
8. Should I get tested too, even if I’m not carrying?
Yes. Always yes. Whether you're the egg source, the intended parent, or just sharing genetics, your STI status matters. Plus, it’s good modeling. If you're asking others to test, walk the walk yourself. You deserve the same peace of mind.
9. Can I use an at-home test for this, or do we need a clinic?
Both work, just depends on your goal. Clinics are great for paperwork, legality, and cryobank rules. But at-home kits are faster, cheaper, and less stressful, especially for pre-screening or known donors. You can always follow up with a lab test if needed.
10. What if they say no or ghost me after I ask?
Then they’ve given you your answer. It might sting, but it’s a gift in disguise. Anyone joining your fertility journey should be able to handle one honest, respectful health question. If they can’t? That’s a boundary, not a loss.
You Deserve Clarity, Not Awkwardness
Choosing to grow your family with the help of a donor or surrogate is brave, beautiful, and complex. You’re already navigating so much: emotions, timelines, bodies, contracts. So let’s make one thing easier:
It is not rude to ask about STI testing. It is responsible. It is kind. It is necessary.
Start the conversation. Use this article as your script, your backup, your reason if you need one. Testing isn’t about fear, it’s about making space for love to grow safely. And love, real love, can handle a test.
How We Sourced This Article: We combined current guidance from leading medical organizations with peer-reviewed research and lived-experience reporting to make this guide practical, compassionate, and accurate. In total, around fifteen references informed the writing; below, we’ve highlighted six of the most relevant and reader-friendly sources. Every external link in this article was checked to ensure it leads to a reputable destination and opens in a new tab, so you can verify claims without losing your place.
Sources
1. Planned Parenthood – STD Testing and Safer Sex
2. What You Should Know - Reproductive Tissue Donation (FDA)
4. 21 CFR Part 1271 Subpart C - Donor Eligibility (eCFR)
5. Guidance Regarding Gamete and Embryo Donation (ASRM, 2024)
About the Author
Dr. F. David, MD is a board-certified infectious disease specialist focused on STI prevention, diagnosis, and treatment. He blends clinical precision with a no-nonsense, sex-positive approach and is committed to expanding access for readers in both urban and off-grid settings.
Reviewed by: Lana Quinn, PA-C | Last medically reviewed: February 2026
This article is for informational purposes and does not replace medical advice.






