Tested Positive Without Having Sex? You’re Not Alone
Quick Answer: Yes, you can get an STD without cheating. Many STDs can lie dormant for months or years, reactivate later, or be transmitted in non-sexual ways. A positive test in a monogamous relationship doesn’t always mean someone was unfaithful.
“How Did This Happen?”: The Confusion of a Positive Test in a Faithful Relationship
Kai, 33, was in a monogamous relationship for four years when he tested positive for HSV-2. “I thought she had cheated on me,” he said. “I confronted her crying. She denied it and I didn’t believe her. But then her OB-GYN told her she had it for years, and probably never knew.”
This is more common than people realize. Many STDs, especially herpes, HPV, and even chlamydia, can live silently in the body. You might never see a symptom. You might carry it for years without a flare-up or issue. Then one day, maybe during a routine screening, or because of unrelated symptoms, you get a test, and it’s positive.
The result? A trauma loop. People feel betrayed, ashamed, angry, or gaslit. But biologically, there are multiple explanations for this experience that have nothing to do with cheating. Let’s break it down.

People are also reading: Does Herpes Always Mean Sores? Here's When It Doesn't
STDs That Can Lie Dormant for Months (or Years)
Some STDs don’t cause noticeable symptoms, or the symptoms are so mild, people mistake them for something else. This allows the infection to sit silently in the body, undetected and unaddressed, until a flare-up happens or testing is finally done.
Table 1. STDs that may remain dormant or asymptomatic for extended periods, leading to delayed diagnoses in monogamous relationships.
This isn’t rare, it’s biology. For instance, CDC data show that many people with genital herpes don’t know they have it because they’ve never had a noticeable outbreak. Similarly, HPV often has no symptoms at all until a pap smear flags abnormal cells.
The truth? Your partner could have had the infection long before your relationship began, and just never knew. Or, less commonly, the infection could be from you, unknowingly. Either way, it’s not proof of betrayal.
Reactivation: When an Old STD Comes Back Without New Exposure
Some STDs, like herpes and HPV, don’t fully “go away.” Once you’re infected, the virus can live in your body for life, reactivating under certain conditions, stress, illness, immune changes, even menstruation.
This means a partner who tested negative years ago or had no symptoms could experience a flare-up long after their last sexual exposure. That reactivation isn’t new cheating, it’s the same old virus waking up.
Sandra, 42, was married for 11 years when she had her first herpes outbreak. “I thought my husband had cheated. But we both got tested. He was positive too, probably from college. I just never had an outbreak until now.”
Herpes latency can be decades-long. The virus lives in nerve cells and reactivates intermittently. A sudden positive result doesn’t mean a new infection, it might mean the virus finally showed its face.
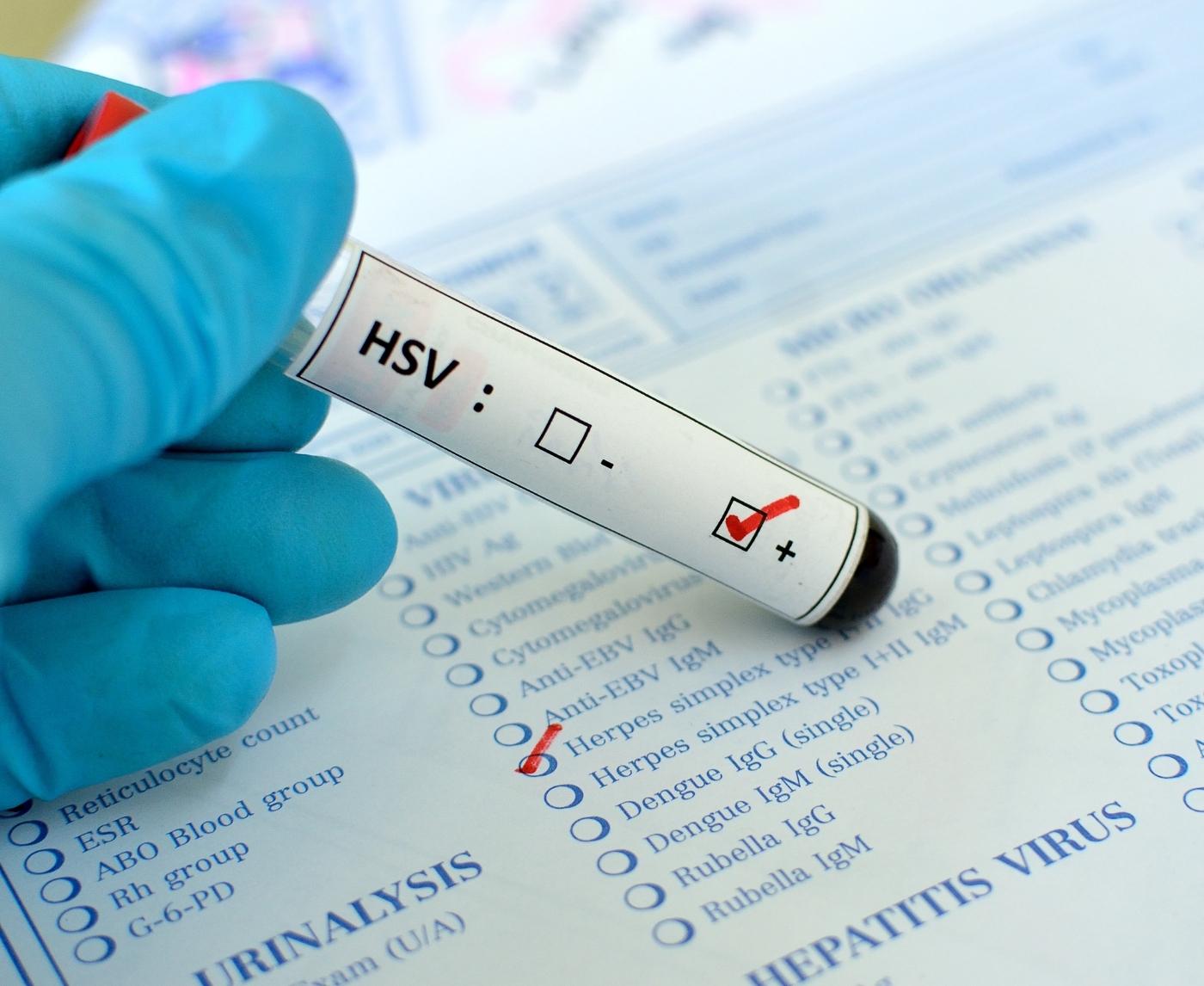
False Positives and Testing Nuances
Another option? The test isn’t lying, but it’s not the full picture either. Some STD tests, especially those that look for antibodies, can sometimes give false positives, especially for herpes and syphilis.
Herpes blood tests (IgG type-specific) can yield confusing results. Some people fall into a “low positive” range that may not reflect an actual infection. That's why most doctors suggest doing confirmatory tests or repeating tests weeks later to make sure the result is correct. The same is true for syphilis, which often uses a two-step test (RPR followed by a treponemal test).
Always follow up with a provider familiar with STD testing. Don’t panic from a single number, context matters. So does lab quality, test timing, and your personal history.
Need a place to start? STD Test Kits offers discreet, clinically reviewed test kits shipped in plain packaging. If you’re sitting on fear or doubt, answers may be a test away.
STDs That Don’t Always Need Sex to Spread
Let’s clear up one of the most confusing truths about sexually transmitted infections: not all of them require “sex” in the way people usually define it. Some STDs can be passed through skin-to-skin contact, sharing personal items, or even from mother to child during birth.
Herpes, for instance, can spread through kissing or oral sex, even without visible sores. HPV is transmitted via skin-to-skin contact and can show up years later without warning. And Trichomoniasis, while usually sexually transmitted, has been found to survive on damp materials like towels or underwear for short periods, especially in warm, moist environments.
Does this mean you can get an STD from a toilet seat? Not likely. But the point is: you can’t always draw a straight line between a positive result and a recent sexual act. Our bodies are messy. Infections are complicated. And not every positive test means betrayal.
According to Mayo Clinic guidance, even sharing sex toys without cleaning them properly can transmit infections. So if either partner had a sexual past before the relationship, even one that seemed “safe”, some risks may still exist.
How Long Can STDs Stay Hidden in the Body?
Different STDs behave differently. Some show up quickly. Others lie in wait. Many people assume that because they’ve been “clean” for years, there’s no way they could test positive later. But some infections don’t follow that timeline.
Table 2. Dormancy and reactivation potential of common STDs, key factors in long-delayed diagnoses.
So what does this mean? It means that even if you and your partner have been monogamous for years, one of you could have carried an infection from before the relationship, and only now is it showing up.
This is especially true for HPV and herpes. You might’ve been infected in your teens or twenties, never showed symptoms, and only now are seeing the results. This isn’t a flaw in your relationship. It’s just virology.
What to Say to Your Partner (Without Breaking Trust)
A positive STD test in a faithful relationship can blow up your trust, or bring you closer. It depends on how it’s handled.
Here’s the reality: your partner might be just as blindsided and scared as you. They might feel accused. They might get defensive. And you might be tempted to scream. But underneath that heat is fear: fear of betrayal, fear of being unclean, fear of being judged.
The best move? Lead with facts, not accusations. Say something like:
“I just tested positive for [X]. I know I haven’t been with anyone else, and I’m scared. Can we talk through what this could mean, together?”
Invite them into the problem. Let them speak. Listen to their experience. And if it helps, involve a provider or therapist to mediate. Testing positive doesn’t have to equal cheating, but it will trigger pain if the conversation starts with blame.
What Now? When to Test, Retest, and Treat
If you’ve tested positive, your next steps depend on the infection, your symptoms, and whether your partner is also tested. Here’s what we recommend:
- Confirm your result. For infections like herpes or syphilis, a second test may be needed to verify accuracy.
- Test your partner. Even if they feel fine, they may be asymptomatic or unaware.
- Treat early. Most STDs are treatable or manageable, and the sooner you treat, the lower your risk of complications or transmission.
- Retest if needed. After treatment, some STDs like chlamydia or gonorrhea require retesting within 3 months to ensure clearance.
If you’re unsure when or how to test, 6‑in‑1 At‑Home STD Test Kit offers discreet testing for multiple infections, with easy-to-read results and no clinic visit required. Peace of mind is one test away.
Couples Who Survived the Shock (And Got Stronger)
There’s a reason this topic is so painful, it hits at the heart of intimacy and trust. But many couples not only survive a surprise STD diagnosis, they thrive afterward.
Jordan and Amina had been married seven years when Amina tested positive for HPV after a pap smear. “I was devastated,” she said. “He believed I cheated. But when he got tested too, he had the same strain. We figured it came from one of us years ago, and only now did it resurface.”
They went to counseling. They cried. But they didn’t split. “We realized the infection wasn’t the betrayal, the assumption was,” Jordan said.
STDs are not moral verdicts. They are biological realities. And facing them with truth, empathy, and science can actually deepen your relationship, not destroy it.

People are also reading: At-Home Chlamydia Test Reviews for 2025: Fast, Private, Reliable
Rebuilding Trust and Sexual Confidence After an STD
A positive STD result doesn’t just shake the medical side of your life, it hits your emotional core. Many couples stop having sex. Some avoid eye contact. Others spiral into cycles of doubt and unspoken resentment. But it doesn’t have to be that way.
Here’s what many trauma-informed therapists recommend: separate the infection from the identity. You are not “dirty.” Your partner is not “a liar.” You are two people navigating a health discovery that, while painful, can be survivable and even transformative.
Sex therapist Laura C., LCSW, says: “The conversation shouldn’t start with shame. It should start with, ‘What do we do with this new information? How do we stay safe, intimate, and honest moving forward?’”
Some people find new ways to be sexual, using condoms, antivirals, or focusing on forms of intimacy that reduce risk during outbreaks. Others pause, talk, and slowly rebuild physical closeness through testing, education, and consent. There’s no one roadmap. But there is a path forward.
How to Manage Recurring Infections in a Monogamous Relationship
Not every STD is a one-time deal. Herpes and HPV can return periodically, even without new exposure. If you’re in a committed relationship, this can feel demoralizing: “We already handled this, why is it back?”
The answer? Viral latency. Some infections don’t leave the body entirely, they go dormant, living quietly in nerve cells or tissues, then reactivate during immune dips or stress. This is normal. It’s not a sign of new cheating. It’s how these infections work.
To reduce flare-ups:
-
Keep an eye on your sleep, stress, and diet.
-
Use antiviral therapy that stops the virus from spreading, like valacyclovir for herpes.
- Stay away from things that you know will set you off, like friction, illness, or times of high stress.
Regular pap smears or anal screenings can check for changes in cells that are caused by HPV. Many strains go away on their own over time. Some people may stay around but never cause problems. Being aware and alert is the key, not panic.
If you’re managing a recurring STD together, routine testing can be a shared ritual rather than a punishment. Consider doing it together, just like any other health check-in. It builds accountability and reduces anxiety.
When Should Couples Retest, and Why?
Retesting isn't just to find new infections. It's about feeling safe, keeping an eye on the viral load, or making sure the treatment worked. A shared retesting timeline can help couples who are getting over a surprise diagnosis feel like they have control again.
This is a general guide:
- After Treatment: Test for chlamydia and gonorrhea again in three months to make sure they are gone.
- For herpes, you don't need to be retested unless your symptoms change or your first test didn't give you a clear answer.
- HPV: After a year, do a pap or anal cytology test again to check for changes in cells.
- If you were recently exposed to HIV, you should get tested at 6 weeks, 3 months, and again at 6 months to be sure.
The 7-in-1 Complete At-Home STD Test Kit from STD Rapid Test Kits offers multi-STD coverage with fast, discreet results, no appointment required.
Whether you’re starting fresh or checking in post-treatment, testing together sends a powerful message: we’ve got this. Together.
Your Relationship Isn’t a Diagnosis
Let’s end with this: A positive STD test doesn’t define your worth, your truth, or your relationship. It’s a medical moment, one with emotional weight, yes, but also with solutions, science, and support behind it.
You’re not the first couple to face this. You won’t be the last. And if you handle it with honesty and informed care, you might walk out of this more connected than ever.
If you're ready to take the next step, even if it's just getting more clarity, check out this option: Essential 6-in-1 At-Home STD Test Kit can offer peace of mind from your own home.
FAQs
1. Can I really get an STD if nobody cheated?
Yes. 100%. It happens more than people realize. Some STDs, especially herpes, HPV, and trichomoniasis, can hang out in your body quietly for years. No symptoms. No drama. Then boom: one flare-up or one routine test and suddenly everyone’s staring at each other like somebody must’ve done something wrong. But the body doesn’t work on relationship timelines, it works on biology.
2. Could this be from before we got together?
Absolutely. This is one of the most common explanations. Many people carry STDs from past partners and only find out years later. If either of you ever had sex before the current relationship (even if it was “protected” or felt safe), that past partner might’ve unknowingly passed something on. It’s not a morality tale, it’s a timeline issue.
3. Why did this show up now, after all this time?
Viruses like herpes and HPV are sneaky. They can lie dormant in your system and then reactivate due to stress, illness, a change in hormones, or literally nothing at all. You could go ten years with no sign, and then suddenly, your immune system dips, and the virus says “Hi again.”
4. Are false positives a thing with STD tests?
Yep. Especially with herpes blood tests and early-stage syphilis tests. Some labs have cutoffs that lead to confusing results, like “low positive” or “equivocal.” That doesn’t mean you’re infected, it means you should double-check with a provider who knows how to interpret that gray zone. One test ≠ gospel.
5. Do I need to worry about towels, toilet seats, or hot tubs?
Mostly, no. Those myths die hard, but they’re mostly bunk. That said, STDs like trichomoniasis can, in rare cases, survive on damp objects like shared towels or swimsuits, though it’s not common. Sex toys, on the other hand? Clean them. Use protection with them. They absolutely can transmit infections between partners.
6. How do I talk to my partner without it turning into World War III?
Start with curiosity, not blame. Try: “I just got this result and I don’t understand it. I haven’t been with anyone else, and I need us to figure this out together.” That opens the door to discussion instead of accusations. You’re scared. They’re probably scared. You’re both human. Let that be the starting point.
7. We’ve been exclusive for years, could we both have it and just never know?
Definitely. That’s especially true for HPV and chlamydia. Most people don’t get tested unless they have symptoms, and some infections don’t trigger symptoms at all. You could both be walking around with the same bug for years and only just now stumble into a test that finds it.
8. Should we both get tested now?
Yes, it’s a good move. Testing as a couple can take the edge off emotionally and helps catch anything that might’ve gone unnoticed. You can do it privately at home with something like a Combo STD Test Kit, or go to a clinic if you’d prefer a provider to walk you through it.
9. Can we still have sex if one of us tests positive?
Generally, yes, a couple of adjustments. Depending on the infection, you may want to consider waiting for treatment, becoming more consistent with condoms, or exploring suppressive medications (like antiviral for herpes). Most people continue a healthy sex life following an STD diagnosis, it’s all about being smarter, not necessarily stopping.
10. Is our relationship doomed?
No. Not even close. What matters more than the test result is how you respond to it, together. Some couples fall apart under the weight of assumptions and silence. Others get stronger by facing it head-on. This can be a turning point, not a breaking point. You’re not broken. You’re not dirty. You’re just… informed.
You Deserve Answers, Not Assumptions
If you've tested positive for an STD but know in your gut that no one stepped out, you're not alone, and you're not wrong to feel confused. The medical world doesn't always explain the nuance of latency, reactivation, and asymptomatic transmission. But that nuance matters.
Relationships don't crumble because of a diagnosis, they crack under the weight of misunderstanding. You now have better information. Use it to test wisely, talk honestly, and treat with care, not blame.
Don’t wait and wonder, get the clarity you deserve. This at-home combo test kit checks for the most common STDs discreetly and quickly.
How We Sourced This Article: We combined current guidance from leading medical organizations with peer-reviewed research and lived-experience reporting to make this guide practical, compassionate, and accurate. In total, around fifteen references informed the writing; below, we’ve highlighted some of the most relevant and reader-friendly sources.
Sources
3. Sexually Transmitted Infections Treatment Guidelines, 2021 | CDC
4. Screening for Genital Herpes | CDC
5. False-positive HIV Test Results | CDC Library
About the Author
Dr. F. David, MD is a board-certified infectious disease specialist who works to stop, find, and treat STIs. He combines clinical accuracy with a straightforward, sex-positive attitude and is dedicated to making his work available to more people, both in cities and in rural areas.
Reviewed by: A. Ruiz, MPH | Last medically reviewed: December 2025
This article is for informational purposes and does not replace medical advice.