When the STD Test Says “Negative” But Your Body Says “Something’s Wrong”
Quick Answer: STD risk can increase after childbirth because of tissue changes, immune shifts, and resumed sexual activity. Burning, unusual discharge, odor, spotting, or pain during postpartum sex may signal infections like Chlamydia, Gonorrhea, Trichomoniasis, or Herpes. Testing is the only way to know for sure.
Why STD Risk Can Increase After Birth, Even in Long-Term Relationships
There’s an assumption that postpartum equals safe. Same partner. Same home. Same life. But sexually transmitted infections don’t follow emotional logic. They follow biology. And postpartum biology is, for a while, more exposed than most people realize.
After delivery, your cervix may remain slightly open for weeks. The uterus is still healing. Vaginal tissue is often thinner because estrogen levels drop sharply after birth, especially if you’re breastfeeding. That thinning changes the vaginal microbiome and pH, which can reduce the natural defenses that usually make it harder for bacteria and viruses to take hold. The CDC’s general guidance on STI transmission emphasizes that mucosal integrity matters, and postpartum tissue is not at full strength yet.
Microtears from vaginal birth, scar sensitivity from C-sections, internal inflammation, and sleep-deprived immune recalibration all contribute. This isn’t about being reckless. It’s about a body that just did something monumental and is still stitching itself back together internally.
And here’s the part nobody says out loud during that six-week clearance: “You can resume sex” does not mean “Your infection risk is the same as it was before pregnancy.” Clearance means your provider doesn’t see active bleeding, major tears, or acute complications. It does not mean your mucosal barrier has fully restored itself or that dormant infections can’t reactivate.
Latent infections such as Herpes (HSV-1 or HSV-2) and HPV can remain asymptomatic for months or even years. According to CDC treatment guidelines, Chlamydia and Gonorrhea are frequently asymptomatic in people assigned female at birth. Pregnancy can suppress immune responses, and the hormonal crash postpartum can allow previously quiet infections to resurface.
This means an infection acquired years ago, by either partner, can flare during that first postpartum sexual encounter. It also means a partner who tested “clean” before pregnancy may no longer be negative if they have not been retested since.

People are also reading: Can an STD Ruin Your IVF Cycle? What Actually Matters
Healing Pain or Hidden Infection? How Symptoms Blur Together
At 2AM, when the baby is finally asleep and your phone screen is glowing against the dark, the line between “normal postpartum healing” and “possible STD symptoms” can feel impossible to draw. Burning during sex? Common. Spotting after penetration? Also common. Odd discharge? That depends on the week.
The problem is that infections often mimic recovery. Trichomoniasis can cause yellow-green discharge and a strong odor, but postpartum lochia can also change color and smell as it fades. Chlamydia may cause mild pelvic discomfort or spotting after sex, which can look like cervical healing. Early Herpes outbreaks can feel like raw tissue or tearing before visible sores appear.
Shira, 28, assumed her discomfort was a small tear that hadn’t healed. “It felt like a bruise inside,” she said. “I didn’t want to seem dramatic.” Two weeks later, a swab confirmed Trichomoniasis. Her partner had no symptoms and had not been tested in years. “I thought we were fine. We’d been together forever.”
Below is a structured comparison to help clarify what deserves a closer look.
None of these symptoms automatically mean you have an STD. But none of them are things you have to ignore either. If symptoms persist beyond a few days, intensify, or come with unusual discharge or odor, testing moves you from guessing to knowing.
When to Test After Having a Baby, Timing Matters
Testing postpartum isn’t about panic. It’s about baseline clarity. If you’ve resumed sex, most experts recommend screening within 4 to 8 weeks after delivery, especially if you notice discomfort, new discharge, or bleeding that doesn’t follow a predictable healing pattern.
The window period, meaning the time between exposure and when a test can reliably detect infection, still applies after birth. According to CDC treatment guidelines, nucleic acid amplification tests (NAATs) for Chlamydia and Gonorrhea can detect infection as early as 5 to 7 days after exposure, but peak accuracy is closer to 14 days or later. Blood-based antibody testing for Herpes may require 12 weeks or more if no active lesions are present.
The table below outlines realistic postpartum testing windows.
If you had sex last week and symptoms start today, testing is still useful. Just understand that a negative result may need confirmation in two to four weeks. Think of it as a checkpoint, not a verdict.
If waiting for an OB appointment feels unrealistic, an option like the 6‑in‑1 At‑Home STD Test Kit allows you to screen for multiple infections discreetly at home. Urine sample. Fingerstick. No speculum. No waiting room. Just answers.
Your Postpartum Immune System Is Recalibrating, And That Matters
Pregnancy shifts your immune system into a carefully balanced state. It has to tolerate a fetus while still protecting you from infection. After delivery, that balance doesn’t instantly snap back. It recalibrates. Hormones drop sharply, especially estrogen, which affects vaginal tissue thickness, lubrication, and microbiome stability.
Research published in infectious disease and obstetric literature shows that estrogen loss postpartum alters vaginal pH and microbial diversity. That shift can create conditions where organisms like Trichomoniasis or bacterial imbalances take hold more easily. When tissue is thinner and drier, friction during sex can create microscopic breaks that increase transmission risk.
Add sleep deprivation, stress hormones, and physical recovery from labor or surgery, and you have a temporary window of vulnerability. This does not mean you are fragile. It means your body is healing in layers, and some of those layers are invisible.
It’s also why postpartum sex can feel raw in ways that are hard to describe. Sometimes that rawness is healing tissue. Sometimes it is inflammation. And sometimes it is infection. The only way to separate those is with testing.
“We Were Both Negative Before the Baby.” Here’s Why That Might Not Be Enough
This question shows up in postpartum forums constantly: If we were both negative before pregnancy, how could an STD show up now?
First, many infections can remain dormant or asymptomatic for extended periods. Herpes can stay silent for years. HPV may not cause visible changes immediately. Chlamydia can persist without symptoms, especially in people assigned female at birth. A negative test years ago does not mean a negative status today.
Second, not every STD panel screens for everything. Routine pregnancy panels often include HIV and syphilis, but not always Trichomoniasis or comprehensive HSV antibody testing unless risk factors are identified. If neither partner has tested recently, there can be blind spots.
Jordan, 35, assumed her relationship history protected her. “We tested before trying for a baby,” she said. “That felt responsible.” But neither of them retested during pregnancy or after. Months later, she developed persistent discharge and cramping postpartum. A swab confirmed Chlamydia. Her partner had been asymptomatic since college. “He wasn’t cheating. He just never checked again.”
Testing postpartum is not an accusation. It’s maintenance. Like checking tire pressure before a long drive. Bodies change. Status can change. Trust and verification can coexist.
“I Thought It Was Just Hormones”
María, 29, had what most would call a smooth birth. Vaginal delivery. Minimal tearing. A supportive partner. At her six-week appointment, her provider said everything looked fine. “You’re cleared,” she was told.
The first time they had sex again, she winced. “It felt like something was scraping a nerve inside,” she said. She told herself it was dryness. She bought lubricant. She tried again. The smell afterward was unfamiliar, sharp but not exactly foul. A week later, pale discharge with a green tint appeared.
“I didn’t think STD,” she said. “I thought I healed wrong.”
Testing revealed Trichomoniasis. Her partner had no symptoms and had not tested in years. According to CDC data, trichomoniasis is one of the most common STIs globally, and many carriers are asymptomatic. María remembers the shame hitting first. “I felt dirty. Like I did something wrong.”
Her midwife reframed it quickly. “This is common. This is treatable. This is not a character flaw.” A short antibiotic course resolved the infection. The harder part was the emotional recovery. “It would’ve been easier if someone had told me postpartum bodies are more vulnerable,” she said. “I wouldn’t have blamed myself.”

People are also reading: Painful Urination in Women: Top Causes Ranked
How At-Home Testing Fits Into Real Postpartum Life
Logistically, clinic visits with a newborn are a puzzle. Coordinating feeding schedules, finding childcare, sitting in waiting rooms with pelvic discomfort and leaking breasts is not exactly conducive to calm decision-making.
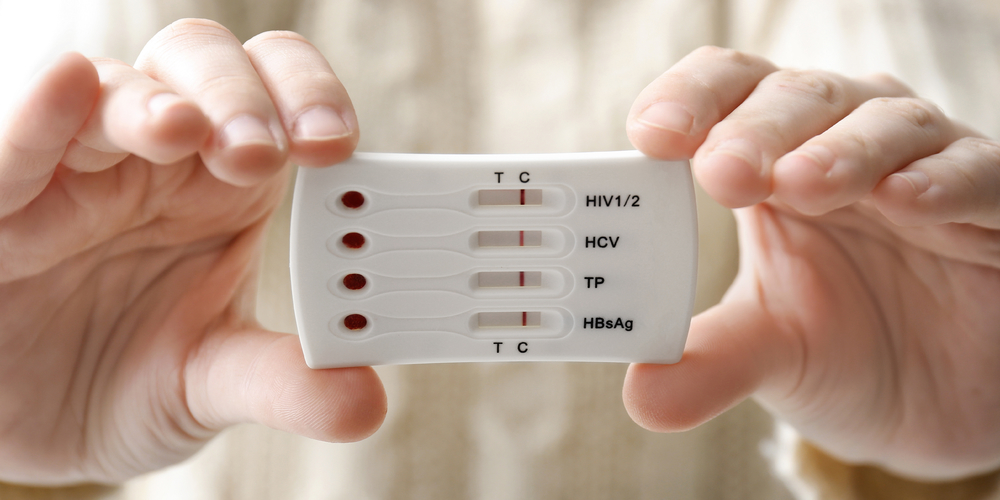
That is where at-home STD testing can bridge the gap between suspicion and confirmation. Most multi-panel kits screen for infections such as Chlamydia, Gonorrhea, Syphilis, HIV, and Trichomoniasis. Collection methods typically involve a urine sample, a vaginal swab, or a small finger-prick blood sample, depending on the infection.
The advantage postpartum is control. You choose the timing. You open the package privately. There is no speculum, no stirrups, and no need to explain your symptoms to a receptionist while rocking a car seat carrier.
If clarity would help you breathe easier tonight, the 6‑in‑1 At‑Home STD Test Kit offers a discreet, comprehensive screening option. Peace of mind does not require a babysitter.
And if a result is positive, you have data. From there, you can pursue confirmatory testing, telehealth consultation, or in-person care. Most bacterial STDs are treated with a short course of antibiotics. Viral infections are manageable with suppressive therapy. Knowledge gives you a plan.
Talking to Your Partner Without Turning It Into a Trial
The postpartum period is already emotionally loaded. Sleep deprivation makes everything sharper. Bringing up STD testing can feel like lighting a match near dry grass. But framing matters.
One approach centers health rather than suspicion. “I’ve been having some symptoms that could just be postpartum stuff,” you might say. “But I’d feel better if we both got tested to rule things out. It’s probably nothing, but I want to be sure.”
Lee, 34, had to navigate this conversation after developing painful urination and small sores. “I was scared she’d think I didn’t trust her,” Lee said of her wife. But her partner admitted she had been having recurrent cold sores and didn’t think much of it. Testing confirmed Herpes. “It was hard,” Lee said. “But facing it together felt stronger than pretending.”
A defensive or resistant response to testing is not proof of guilt. It is often fear. But sexual health conversations are part of adult intimacy, especially after major life events like childbirth. Framing the conversation around mutual protection keeps it collaborative.
If You Test Positive: The First 48 Hours
Testing positive postpartum can feel like the ground shifting under your feet. You may be holding your baby while staring at a result that makes your stomach drop. First: breathe. Most STDs are treatable. Many are curable. All are manageable.
Bacterial infections like Chlamydia, Gonorrhea, and Trichomoniasis are typically treated with antibiotics. According to CDC treatment guidelines, adherence to the prescribed regimen and partner treatment are critical to prevent reinfection. Viral infections such as Herpes require a different strategy, often including antiviral medications to reduce outbreak frequency and transmission risk.
If you are breastfeeding, many standard treatments are considered compatible with lactation, but always confirm with your healthcare provider. Organizations like WomensHealth.gov and the CDC provide guidance on STI treatment during breastfeeding.
The next steps usually include notifying your partner, completing treatment, and retesting at the recommended interval to ensure resolution. Testing positive is not the end of intimacy. It is the beginning of informed decisions.
Retesting After Postpartum Exposure, When One Test Isn’t the Final Word
A negative result can feel like oxygen. A positive one can feel like collapse. But in both cases, timing still matters. Postpartum testing often requires a second look, especially if the first test was taken early in the window period.
If you tested within the first week after sex and your result was negative, that does not always mean you are in the clear. Infections like Chlamydia and Gonorrhea may not reach detectable levels until closer to 14 days post exposure. Blood-based testing for Herpes antibodies can take 12 weeks or longer if no active lesions are present.
Retesting is not paranoia. It is confirmation. And postpartum, when symptoms overlap with healing, confirmation is powerful.
If you were treated for a bacterial STD, most guidelines recommend retesting approximately three months later to ensure no reinfection has occurred. Reinfection is more common than people think, often because a partner was not treated at the same time or because sexual activity resumed before treatment was complete.
Think of postpartum testing as a two-step process when needed: initial screening, then follow-up at the optimal window. That rhythm reduces false reassurance and unnecessary panic.
Reducing False Negatives and Misreads at Home
At-home testing is accurate when used correctly, but like any diagnostic tool, timing and technique matter. Postpartum fatigue is real. Reading instructions while rocking a baby is not ideal. Slow down. Give yourself twenty focused minutes.
For urine-based testing, avoid testing with your first urination of the day unless instructions specify otherwise. Follow collection guidelines carefully. For fingerstick tests, ensure hands are warm to improve blood flow and fill lines properly to avoid invalid results.
Faint lines can cause spirals. A faint line is not “almost negative.” In most rapid tests, any visible test line in the designated area indicates a reactive result. If a line appears where it should not, or if control indicators fail, the test is invalid and should be repeated.
If confusion lingers, consider confirming through a laboratory-based test. Mail-in lab kits or clinic NAAT testing often provide the highest sensitivity for bacterial infections. The goal is clarity, not stubbornly sticking to one method.
Your result should empower you. If it doesn’t feel clear, that’s a sign to retest, not to ignore.
When Postpartum Healing Truly Is Just Healing
Not every uncomfortable postpartum experience is an STD. Vaginal dryness is common, especially with breastfeeding, because estrogen levels remain low. Lubrication may be reduced for months. Tender scar tissue can make certain positions uncomfortable. Pelvic floor muscles may feel tight or strained.
Lochia transitions from bright red to pink to yellow-white over several weeks. Mild odor can occur as blood and tissue clear. Occasional spotting after sex may reflect cervical sensitivity rather than infection.
The key differences often lie in persistence and pattern. Infection-related symptoms tend to worsen or stay consistent rather than gradually improve. Discharge that becomes distinctly green, frothy, or strongly foul smelling deserves evaluation. Burning with urination that persists beyond a day or two is worth testing. Visible sores, blisters, or ulcers are never “just hormones.”
If something changes suddenly after sex, especially if it was not present before penetration resumed, pay attention. Postpartum healing should trend toward better, not sharper or stranger.
The Emotional Weight of Postpartum STD Fear
There is a particular kind of shame that can settle in after childbirth. You are supposed to be glowing. Grateful. Adjusting. When something sexual feels wrong, it can feel selfish to prioritize it. When STD fear enters the picture, that shame multiplies.
Many postpartum people tell us they delayed testing because they were afraid of what it would imply. Afraid it would suggest infidelity. Afraid it would confirm something permanent. Afraid it would make them look irresponsible at a time when they are trying so hard to be everything for everyone.
Testing is not an admission of guilt. It is an act of protection. It protects your body. It protects your partner. It protects your future fertility. Untreated Chlamydia and Gonorrhea, according to CDC data, can lead to pelvic inflammatory disease, which may impact fertility and cause chronic pelvic pain. Postpartum is not immunity against those complications.
You just carried and delivered a human. You are allowed to demand clarity about your own health.

People are also reading: 7-in-1 Complete At-Home STD Test Kit
Making a Clear Decision Without Spiraling
If you are unsure whether to test, walk through this mental checklist calmly.
If sex feels different but gradually improves, and there is no unusual discharge, odor, sores, or persistent burning, lubrication and time may be enough. If symptoms are intensifying, staying the same for more than a few days, or clearly linked to sexual activity, testing moves from optional to wise.
If you or your partner have not tested since before pregnancy, and sex has resumed, establishing a postpartum baseline is reasonable even in the absence of symptoms. That baseline reduces future anxiety. It prevents late-night Google spirals. It lets you reenter intimacy with confidence rather than hesitation.
If you are still debating at 1AM, that hesitation itself is information. Peace of mind matters. A discreet test ordered from home can turn uncertainty into a plan. You can start at STD Test Kits and choose the panel that fits your situation.
What Protecting Yourself Looks Like Going Forward
Postpartum sexuality is not a return to “normal.” It is a new chapter. Protection might mean lubricant for dryness. It might mean condoms while waiting for confirmatory testing. It might mean mutual retesting every year or after any new exposure.
It can also mean vaccines where applicable. HPV vaccination, if not already completed, remains an important preventive tool for many adults within recommended age ranges. Discuss eligibility with your provider.
Protection is not about suspicion. It is about maintenance. Just like scheduling pediatric appointments, you can schedule your own sexual health check-ins.
If you want a comprehensive screen that covers multiple common infections in one step, the Essential 6-in-1 At-Home STD Test Kit allows you to test discreetly and quickly. Answers first. Then decisions.
FAQs
1. Be honest. Can I really get an STD from my long-term partner after having a baby?
Yes. And no, that doesn’t automatically mean someone cheated. Infections like Herpes and HPV can sit dormant for years and flare when your immune system dips, and postpartum is a perfect storm for that. Add tissue changes and hormonal shifts, and something that stayed quiet for a decade can suddenly introduce itself. It’s biology, not betrayal.
2. Sex just feels uncomfortable. How do I know if it’s dryness or something more?
Dryness usually feels like friction and improves with good lubricant and patience. Infection tends to linger or escalate. If you’re noticing burning that sticks around after sex, discharge that looks unfamiliar, a smell that makes you pause, or pain that feels sharp instead of tender, that’s your cue to test. Healing improves. Infections stall or intensify.
3. My discharge looks weird. But postpartum discharge is weird, right?
Yes, lochia can be unpredictable. It shifts colors and textures as your uterus heals. But here’s the difference: normal postpartum discharge fades over time. It doesn’t suddenly turn bright green, frothy, or strongly fishy weeks after slowing down. If your nose wrinkles or the pattern changes suddenly after sex, investigate. Your body is talking.
4. I had sex last week. Is it too soon to test?
Maybe. For Chlamydia and Gonorrhea, five to seven days can catch early infection, but two weeks is more reliable. If anxiety is eating you alive, test now, then retest at the two-week mark if needed. Think of it as a checkpoint, not a final verdict.
5. What if I feel completely fine?
That’s the tricky part. Many STDs are asymptomatic. Chlamydia is especially famous for doing damage quietly. Postpartum testing isn’t only about symptoms. It’s about establishing a baseline so you’re not second-guessing every twinge for the next six months.
6. I’m breastfeeding. Can treatment mess that up?
Most common antibiotic treatments for bacterial STDs are considered compatible with breastfeeding. Your provider can confirm specifics, but in most cases, treating the infection protects both you and your baby more than avoiding medication does. Untreated infection is the bigger risk.
7. This feels awkward to bring up. How do I even start that conversation?
Lead with health, not suspicion. Try: “Postpartum bodies are weird, and I’ve had some symptoms. I’d feel better if we both tested just to rule things out.” You’re not accusing. You’re protecting. If your partner values your health, they’ll meet you there.
8. What if the test is positive? I don’t think I can handle that right now.
You can. It will feel heavy for a moment. Then it becomes a plan. Most bacterial infections are cured with antibiotics. Viral infections like Herpes are manageable and incredibly common. A positive result is not a life sentence. It’s a starting point for treatment and honesty.
9. Why didn’t my OB automatically test me at my postpartum visit?
Because postpartum appointments focus on bleeding, healing, contraception, and mental health. STD panels aren’t always routine unless risk factors are discussed. That doesn’t mean you don’t deserve one. It just means you sometimes have to ask, or choose a discreet at-home option.
10. Do I really need to test if we’re “low risk”?
Low risk isn’t zero risk. If you haven’t tested since before pregnancy and sex has resumed, that’s reason enough. Testing isn’t dramatic. It’s maintenance.
You Just Had a Baby. You Still Deserve Certainty.
Postpartum life is loud, exhausting, and full of invisible adjustments. When sex feels off, when discharge changes, when something inside you says this isn’t just hormones, that voice deserves attention. STD risk does not pause because you gave birth. And testing is not an accusation. It is maintenance.
If you want to stop guessing and start knowing, the Women’s 10‑in‑1 At‑Home STD Test Kit screens for multiple common infections discreetly from home. No waiting room. No awkward explanations. Just clarity, so you can focus on healing, bonding, and reclaiming intimacy on your own terms.
How We Sourced This Article: This guide was developed using current CDC STI treatment guidelines, postpartum care standards from ACOG and major medical institutions, peer-reviewed infectious disease research, and lived-experience reporting to reflect real postpartum concerns. Approximately fifteen references informed the analysis. Below are six of the most authoritative and reader-accessible sources. All links were verified to ensure accuracy and credibility.
Sources
1. CDC Sexually Transmitted Infections Treatment Guidelines
2. Sex After Pregnancy: Set Your Own Timeline – Mayo Clinic
3. Sexually Transmitted Infections, Pregnancy, and Breastfeeding – WomensHealth.gov
4. Optimizing Postpartum Care – ACOG
5. Optimizing Postpartum Care | ACOG
About the Author
Dr. F. David, MD is a board-certified infectious disease specialist who focuses on preventing, diagnosing, and treating STIs. He combines clinical accuracy with a straightforward, sex-positive approach and fights for testing options that are easy to get and don't involve judgment for people of all ages.
Reviewed by: A. Hill, NP-C | Last medically reviewed: February 2026
This article is for informational purposes and does not replace medical advice.