HIV Rapid Test Errors and Faint Lines: How to Know What’s Real
Quick Answer: UK health experts warn that STIs like chlamydia and gonorrhea tend to surge over the festive season due to increased casual sex and lowered condom use. At-home testing offers a private, fast way to detect infections early, especially if you’ve had unprotected sex or multiple partners during the holidays.
Who This Guide Is For (And Why It Matters)
Maybe you woke up the morning after a Christmas party next to someone you didn’t plan on sleeping with. Maybe you had a spontaneous hookup while visiting family, or reconnected with an ex for old time’s sake. If any of this feels familiar, you're not alone. The holiday season is a peak time for risky sex, often involving alcohol, late nights, and forgotten condoms.
Even if you feel fine right now, STIs don’t always come with obvious symptoms. And with many clinics closed or booked out over the holidays, getting tested can feel impossible. That’s where at-home kits come in. This guide is for anyone who had sex during the festive season and wants to know when to test, what kind of test to use, and how to stay safe without shame. Testing isn’t just about you, it’s how we protect everyone we sleep with, now and in the future.

People are also reading: Hepatitis B Window Period: When Early Testing Can Miss It
What Actually Counts as an STD Test?
A real STD test isn’t just someone “taking a look.” It’s a medical test that detects the presence of bacteria, viruses, or parasites that cause infections like chlamydia, gonorrhea, syphilis, herpes, HIV, and trichomoniasis. These are usually done through urine samples, vaginal or throat swabs, or a small amount of blood. Each test looks for specific pathogens using different methods, like nucleic acid amplification tests (NAAT), rapid antigen tests, or antibody screenings.
At-home testing kits use the same lab-grade science used in clinics. Some kits give rapid results in minutes. Others require mailing your sample to a certified lab and waiting a few days for results. Both options are valid. Both are private. And both can help you act quickly if something shows up. You can explore discreet testing options here at STD Test Kits, including the popular Combo STD Home Test Kit that screens for multiple infections at once.
Window Periods: What to Know for Each STD
This is where things get hard. You could test today and not get an infection from yesterday's test. There is a "window period" for every STD. This is the time between when you are exposed to the disease and when a test can reliably find it. If you're anxious and want answers right away, testing too soon can give you a false negative. But knowing when to say what helps you avoid false comfort.
Figure 1. Window period and accuracy table for common STDs. Always check the timing before testing to avoid false negatives.
Rapid Test vs Lab Test: Pros, Cons, and Tradeoffs
On December 27th, someone might be sitting in their car outside their parents’ house, holding a rapid test they picked up online. A few drops of blood. Ten minutes. A sigh of relief, or a moment of clarity. That’s the power of fast, private information.
Rapid at-home tests are great for quick checks, especially for HIV, syphilis, or trichomoniasis. But for infections like chlamydia and gonorrhea, lab-based NAAT tests are considered more accurate. Mail-in kits combine the privacy of at-home collection with the accuracy of lab processing. And if you have serious symptoms, or a positive result, you may still want to follow up with a provider.
Figure 2. Comparing testing methods by privacy, accuracy, and timing. Choose what works best for your situation and stress level.
When to Test After Exposure
If it’s been less than five days since you had unprotected sex at that Christmas party or New Year’s Eve hookup, testing might be too soon for most infections to show up. But that doesn’t mean you should do nothing. If symptoms show up early, burning, unusual discharge, or sores, test immediately. Otherwise, waiting until the window period gives you the most reliable result.
If it’s been between 7 and 14 days, this is the sweet spot for testing for chlamydia, gonorrhea, and trichomoniasis. Even if your result is negative now, it’s smart to retest after three weeks if you’re still worried. For HIV and syphilis, you may need to wait a bit longer for accurate results, but testing now can establish a helpful baseline.
If it’s been over two weeks, test now. You’re well into the window period for most common STDs, and your result will be more reliable. One reader shared this: “I tested five days after a New Year’s one-night stand. It came back negative. But I still felt off. I retested at three weeks and found out I had chlamydia.” That second test likely prevented a longer infection and further spread.
If your head keeps spinning, peace of mind is one test away. Order a discreet combo test kit here to screen for multiple infections at once, all from home.
Do You Need to Retest? Here’s How to Know
If you tested too early, or if your exposure happened during the high-risk window around the holidays, retesting gives you a second line of defense. Retest at the end of the recommended window period, even if your first test was negative. This is especially true if you’re having new or multiple partners, have any symptoms, or didn’t use protection every time.
If you were treated for an STD recently, like chlamydia or gonorrhea, don’t test again right away. Dead bacteria can still show up and cause a false positive. Wait three to four weeks post-treatment to confirm you’re clear. If you weren’t treated, or if your partner tested positive, retesting around the 30- to 45-day mark makes sense.
Privacy, Shipping, and Discreet Support
Ordering an STD test during the holidays doesn’t have to be awkward. Kits arrive in plain packaging, no branding, no health-related labels, no surprises. Most ship within one business day, even during peak holiday periods. Some customers receive theirs in as little as 48 hours, depending on location and courier speed.
Inside, instructions are clear, and everything is self-contained. No awkward pharmacy runs. No clinic waiting rooms. And no one else sees your results unless you choose to share them. It’s your sexual health, your pace, your privacy.
If you’re traveling or staying with family, plan ahead. Ship to a trusted address or use a locker pickup option if available. Most people test in a bathroom or bedroom with 10 minutes to spare. One customer wrote, “I took my test in my old childhood bedroom while my family was watching Elf downstairs.” Life doesn’t stop for sexual health, and neither should you.
What If You Test Positive?
It’s not the end of the world. A positive test during the holidays can feel extra heavy, but the truth is: most STDs are treatable. And getting a result means you’re already doing the right thing. You’ve taken control of your health, and that’s powerful.
Start by confirming the result. Some infections, like herpes or syphilis, may require a follow-up test or clinical diagnosis. From there, treatment is usually straightforward, antibiotics for bacterial infections, or antivirals and ongoing management for viral ones. If you don’t have a regular doctor, telehealth options and sexual health clinics are still available in many places, even during holiday hours. The Planned Parenthood site can help you find care nearby.
And yes, you’ll need to tell your partners. It’s not easy. But anonymous notification tools exist, and many people will appreciate your honesty. Imagine sitting in your car after seeing a positive test. Your first reaction might be panic. But then you breathe. You send the message. And instead of shame, you feel relief. You’ve done the responsible thing.
At-Home Testing, Your Secret Weapon
The holidays amplify everything, connection, loneliness, desire, spontaneity. For some, it’s the time of year they reconnect with old flames. For others, it’s a string of holiday parties that blur into hookups and hazy mornings. In all that celebration, conversations about protection and STIs tend to vanish. But just because it’s common doesn’t mean it’s safe.
That’s why at-home STD testing matters more than ever right now. Clinics are often closed, phones go unanswered, and shame blocks even the best intentions. But your body doesn’t care what day it is. If you were exposed during the holidays, waiting until things “settle down” could mean missing your window, or passing something along unknowingly.
At-home kits break the cycle. You don’t need an appointment, you don’t need to explain yourself, and you don’t need to wait. Just order, collect, and test. Privacy, speed, and power, all in your hands.
Figure 3. Common post-holiday testing scenarios and how at-home kits provide real-time control and reassurance.
This isn’t about panic. It’s about patterns, and breaking them. If STIs spike every December, we don’t need more judgment. We need more access. More privacy. More people taking initiative when the system is slow, silent, or stigmatizing. That’s why we built resources like the STD Risk Checker Quiz, so you can assess your risk before you even click “order.”

People are also reading: Negative STD Test, Still Have Symptoms? Here's What Could Be Going On
Still unsure when to test? You're not alone.
One of our most-read articles is this detailed breakdown of STD testing windows by infection. It helps you pinpoint when a test will be most accurate, based on the day of exposure and the infection type.
Information should be your safety net, not a gatekeeper. So here’s what we know: STIs rise after Christmas. Young people are most affected. Clinics are slammed or closed. But you don’t have to be stuck. The solution isn’t just testing, it’s access to testing that meets you where you are, emotionally and physically.
Whether it’s a morning of regret, a week of worry, or a partner asking “Should we test?”, you can take the next step today. Order your discreet at-home combo kit and stop wondering.
FAQs
1. Is there really a rise in STIs every December?
Yes. Health agencies in the UK and US have both observed seasonal surges in chlamydia, gonorrhea, and other infections during the holidays. The spike is linked to increased casual sex, alcohol use, lowered condom use, and delayed access to testing. This year’s warnings follow consistent multi-year data trends.
2. Why do STDs not show up on tests right away?
After exposure, the body needs time to develop enough viral material, bacteria, or antibodies to be detectable. This period, called the “window period”, is different for every STD. Testing too early can give false reassurance, so it’s critical to understand when accuracy peaks. For a breakdown, see our full guide on window periods by infection.
3. How do I know if I should test at all?
If you had unprotected sex, changed partners recently, experienced symptoms, or just feel uneasy, testing is the only way to be sure. You can also use our STD Risk Checker Quiz to gauge whether you should test now, later, or not at all.
4. Can I get accurate results with an at-home kit?
Yes. At-home tests employ the same type of testing used at clinics, such as NAAT, antigen, and antibody tests.The trick is to take the test at the correct time during the testing window and purchase the test kits from reliable vendors such as STD Rapid Test Kits.
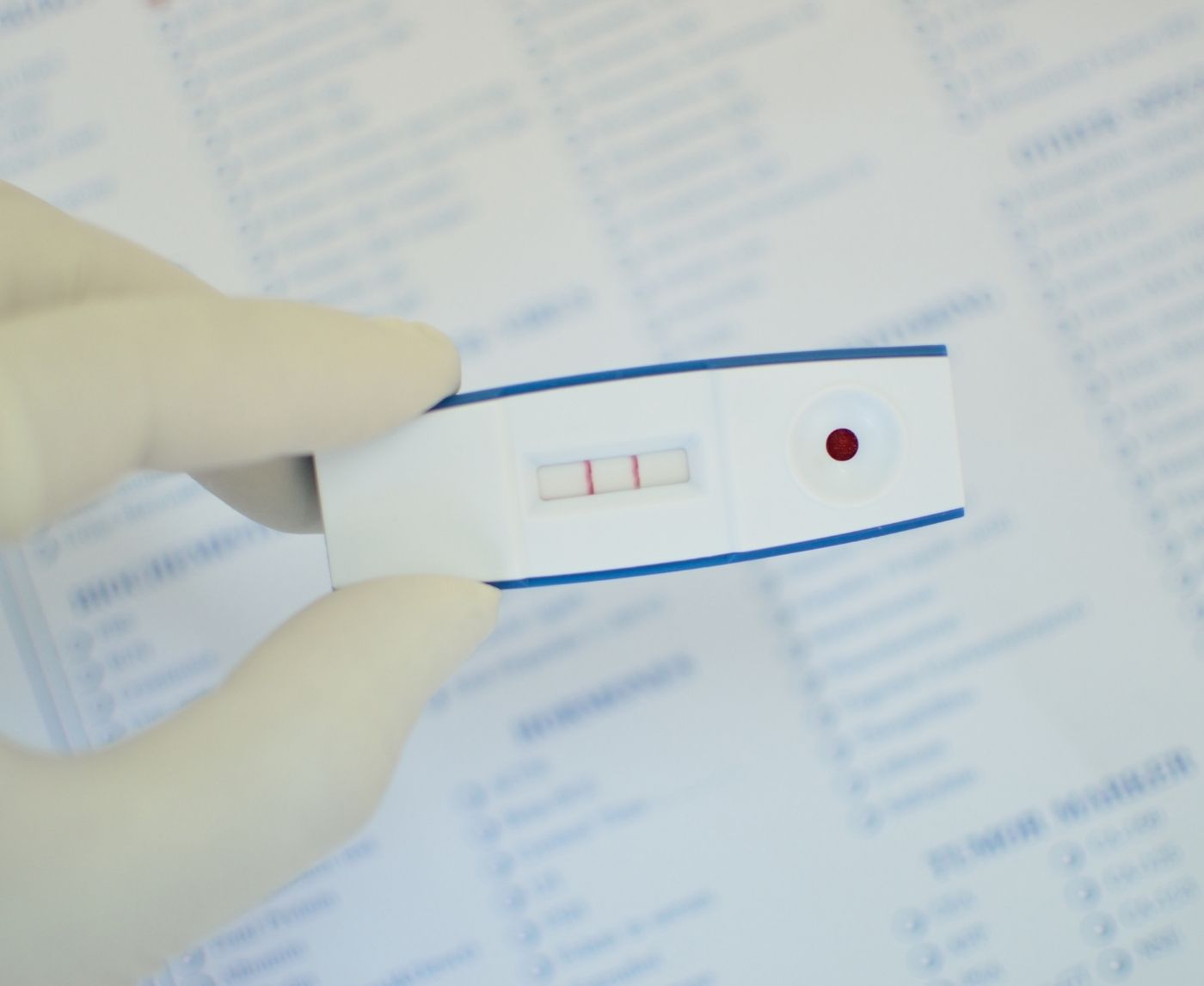
5. Are faint lines on a test still positive?
They can be. Many rapid test cassettes count any visible test line, no matter how faint, as a positive. Always check the instruction sheet, and if you're unsure, consider a mail-in lab kit or follow-up test for confirmation.
6. What if my partner refuses to test?
That’s tough, but your health still comes first. Test yourself, and if you test positive, you can choose to notify them directly or anonymously using online services. You can’t control their reaction, but you can protect your body and future partners.
7. Can I use an STD test while I’m on antibiotics?
If you’re already on treatment, the test may return a false negative, especially if the bacteria is being cleared. If possible, wait at least 21 days after finishing antibiotics before retesting.
8. Do I need to test again if I already tested in early December?
If you’ve had new partners, symptoms, or unprotected sex since that test, yes, you should retest. A test from three weeks ago doesn’t account for what happened last night or over the holiday weekend.
9. What happens if I ignore a positive result?
Untreated STDs don’t go away. They can lead to pelvic inflammatory disease, infertility, chronic pain, and higher HIV risk. But the good news is: most are easily treatable. Acting fast makes all the difference.
10. How discreet is shipping from STD Rapid Test Kits?
Extremely. Packages arrive in plain, unbranded envelopes with no health-related identifiers. Nothing on the outside reveals the sender or contents. It’s privacy-first, by design.
Still Worried? Here’s Your Next Move
There’s a reason you’re still reading. Maybe something happened over the holidays that didn’t sit right. Maybe you’ve been refreshing your symptom search since Christmas. Or maybe you just want to stop carrying the “what if” into the new year. Whatever brought you here, you deserve clarity, and you don’t have to beg a clinic for it.
At-home testing isn’t second-best. It’s a smart, safe, medically backed option when time, privacy, or emotions make everything else harder. If you’ve had unprotected sex, changed partners, felt off, or just want peace of mind, this combo test kit gives you answers without the wait or the awkwardness. No judgment. No pressure. Just results, on your terms.
Test now. Breathe sooner.
How We Sourced This Article: We combined current guidance from leading medical organizations with peer-reviewed research and lived-experience reporting to make this guide practical, compassionate, and accurate. In total, around fifteen references informed the writing; below, we’ve highlighted six of the most relevant and reader-friendly sources. Every external link in this article was checked to ensure it leads to a reputable destination and opens in a new tab, so you can verify claims without losing your place.
Sources
1. NHS: Sexual Health Overview
2. Planned Parenthood: Safer Sex & STDs
3. Sexually Transmitted Infections | Travelers’ Health | CDC
4. Sexually Transmitted Infections (STIs) | WHO
5. Sexually Transmitted Infections Treatment Guidelines | CDC
About the Author
Dr. F. David, MD is a board-certified infectious disease doctor who focuses on preventing, diagnosing, and treating STIs. He combines clinical accuracy with a straightforward, sex-positive approach, and he wants to make it easier for readers to get to know him in both urban and rural areas.
Reviewed by: J. Harris, MPH | Last medically reviewed: December 2025
This article is for informational purposes and does not replace medical advice.