Which STD Test Do I Need Based on My Symptoms?
Quick Answer: A high-risk HPV diagnosis means you’ve tested positive for a strain associated with cancer risk, like HPV 16 or 18. It doesn’t mean you have cancer now, but you’ll need monitoring, possible further testing, and proactive protection strategies.
Who This Guide Is For (And Why It Matters)
If you’ve tested positive for high-risk HPV, this article is for you. Whether you’re already freaking out or trying to stay chill until your doctor calls back, you deserve clear, honest answers. You might be:
- Someone who just got an abnormal Pap or anal cytology result,
- A person living with HIV or immunosuppression who’s been told to monitor HPV more closely,
- Or just someone curious about the cancer risks no one warned you about in sex ed.
We wrote this guide to walk you through exactly what a high-risk HPV diagnosis means, and what it doesn’t. It’s not a sentence. It’s not even a disease in itself. It’s a warning light. And catching it early gives you a powerful advantage.

People are also reading: When to Retest for Chlamydia: A Guide to Preventing Reinfection
Understanding the Difference: High-Risk vs Low-Risk HPV
There are over 100 strains of HPV, but not all of them carry the same risk. Low-risk HPV types (like HPV 6 and 11) are linked to genital warts, uncomfortable, yes, but not dangerous. High-risk HPV strains (like HPV 16, 18, 31, and others) are different. They have the ability to change the DNA of your cells over time, especially in the cervix, anus, penis, vulva, or throat. If left unchecked, those changes can lead to cancer.
According to the CDC, HPV types 16 and 18 cause the majority of HPV-related cancers, including:
Figure 1. Cancers associated with high-risk HPV strains and their most common types.
Why Most High-Risk HPV Infections Don’t Lead to Cancer
Here’s the truth your diagnosis may not have told you: your immune system clears most HPV infections on its own. According to the World Health Organization, over 90% of HPV infections clear within two years. The problem is when they don’t. Persistent infection with a high-risk strain is what leads to cellular changes, and that’s what screening tries to catch.
Think of HPV like a spark. It doesn’t automatically start a fire. But if it lingers in the right conditions, immunosuppression, untreated dysplasia, poor follow-up, that spark can become a flame. That’s why doctors recommend regular Pap smears, HPV genotyping, or anal cytology, depending on your risk profile and anatomy.
What Happens After a High-Risk HPV Result?
The most frustrating part of a high-risk HPV diagnosis is that nothing feels immediate. There’s rarely pain, rarely a pill, rarely a clear “fix this now” moment. Instead, what comes next is surveillance. That word alone can feel ominous, but in medicine, surveillance is power. It means you’ve caught something early enough to watch it before it causes harm.
What happens next depends on where HPV was detected and what your screening showed. For some people, it’s a repeat test in 12 months. For others, especially those with abnormal cells, it means additional procedures designed to look closer, not because cancer is present, but because prevention works best when changes are caught early.
If HPV Was Found on a Cervical Test
If your high-risk HPV result came from a Pap smear or HPV test of the cervix, your provider is looking for signs of cervical dysplasia. Dysplasia means abnormal cell changes, not cancer. These changes are graded based on severity, and most never progress if they’re monitored correctly.
You may be referred for a colposcopy, which allows a clinician to examine the cervix with magnification and take small biopsies if needed. Many people describe the anxiety before the appointment as worse than the procedure itself. One patient told us:
“I spent two weeks convinced my life was over. The biopsy came back mild, and now I just check in once a year.”
The key thing to understand is that time is on your side. Cervical cancer from HPV usually takes many years to develop. Screening exists precisely because it gives you a long runway to intervene.
If HPV Was Found in the Anal Area
High-risk HPV in the anal canal is still widely misunderstood, and because of that, it’s often under-screened. Anal HPV can affect people of any gender or orientation, though rates are higher among men who have sex with men, people living with HIV, and those with weakened immune systems.
If your provider is concerned, they may recommend an anal Pap test or refer you for high-resolution anoscopy. These tests look for anal dysplasia, which, just like cervical dysplasia, can be monitored or treated before cancer develops. Early-stage changes are highly manageable when they’re identified.
This is where early detection saves lives. Anal cancer is rare, but it is increasing, and persistent high-risk HPV is the main driver. Knowing your status allows you to step out of the dark and into informed care.
Understanding Precancer: Dysplasia Is Not Cancer
One of the most common mistakes people make after a high-risk HPV diagnosis is assuming the worst. Dysplasia sounds scary, but it’s not cancer. It’s a spectrum of cell changes that signal risk, not inevitability.
Mild dysplasia often resolves on its own. Moderate changes may require closer follow-up. Severe dysplasia is treated to prevent progression. None of these stages mean cancer is present. They mean your body raised its hand and said, “Pay attention here.”
A clinician once explained it this way: “Cancer is the house fire. Dysplasia is the smoke detector going off.” Listening to that alarm is what keeps the fire from ever starting.

People are also reading: When Travel Turns Risky: How Soon You Should Test After Sex Abroad
How to Protect Yourself After a High-Risk HPV Diagnosis
Protection after a positive HPV result isn’t about blame or regret. It’s about stacking the odds in your favor. That starts with follow-up testing, but it doesn’t end there. Supporting your immune system, reducing reinfection risk, and staying engaged with screening all matter.
Using condoms consistently can reduce HPV transmission and reinfection, even in long-term relationships. Quitting smoking is another major protective step, tobacco use weakens local immune defenses and increases HPV persistence. These changes don’t erase the virus overnight, but they reduce the conditions that allow it to linger.
If you haven’t been vaccinated against HPV, talk to your provider. Even after infection, the vaccine can protect against strains you haven’t encountered yet and may reduce future risk.
Should You Test Again? Timing Matters
HPV testing is not like testing for bacterial infections. You’re not looking for immediate clearance, you’re looking for trends. Most providers recommend repeat testing at set intervals, often 12 months, to see whether the virus has cleared or persisted.
This waiting period can feel unbearable. Many people test too often, hoping for reassurance, only to feel more anxious when results don’t change right away. Persistence doesn’t mean failure. It means your immune system is still working through it.
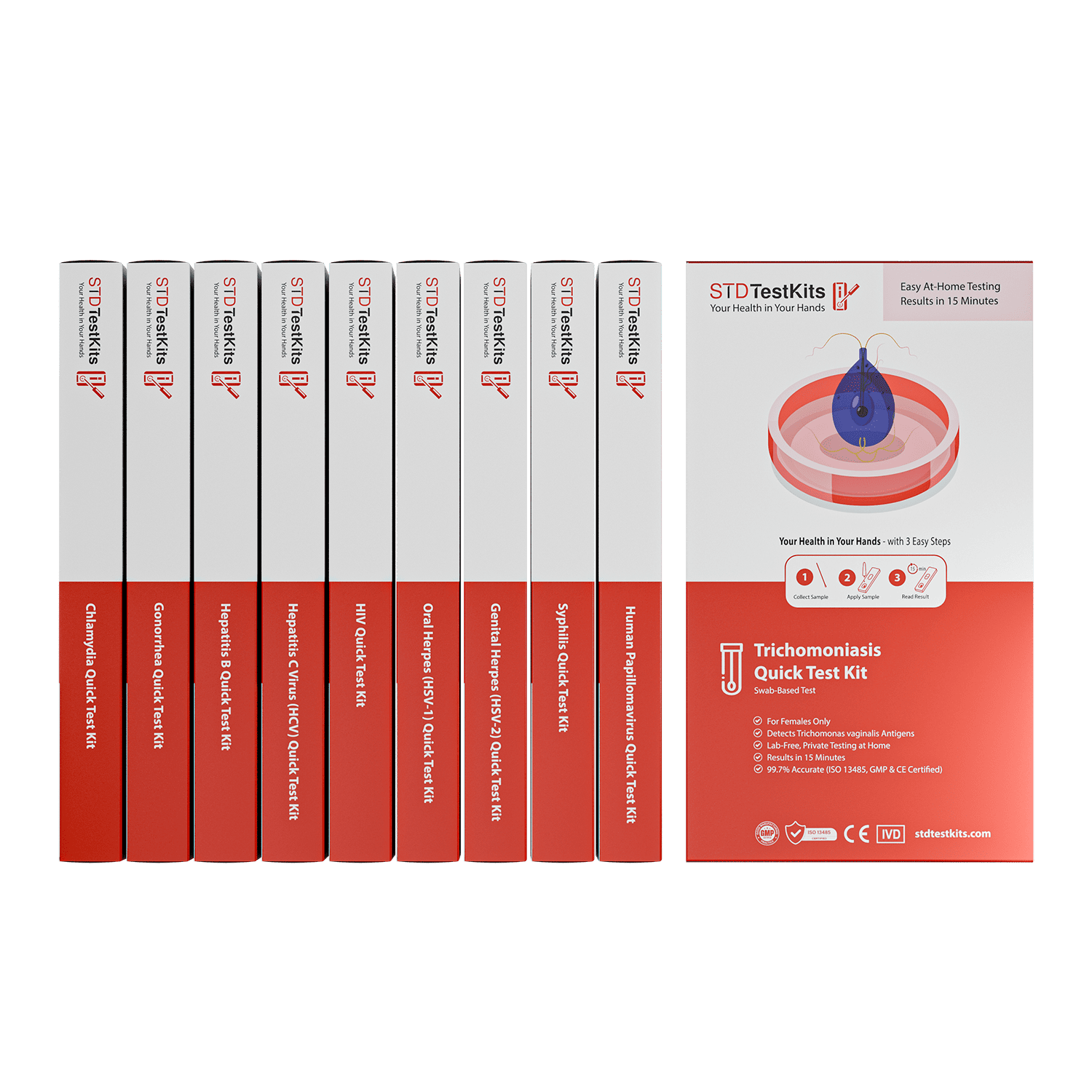
If you’re monitoring from home or want discreet options to stay proactive, tools like at-home HPV screening kits can help you stay engaged without constant clinic visits. You can explore discreet testing options at STD Test Kits if privacy or access is a concern.
Talking to Partners Without Panic
Telling a partner about high-risk HPV can feel harder than the diagnosis itself. There’s fear of blame, misunderstanding, or rejection. The reality is that HPV is incredibly common, often shared unknowingly, and impossible to trace to a single encounter.
One woman described it this way: “I expected anger. Instead, my partner said, ‘Okay, what do we do now?’ That was the moment I stopped feeling alone.” A good conversation focuses on shared care, not fault. HPV doesn’t mean infidelity, and it doesn’t mean someone did something wrong.
Framing the conversation around prevention and monitoring, not danger, can change everything.
When to Seek Immediate Medical Care
Though HPV itself is asymptomatic, there are some symptoms that should not be ignored. If you have unexplained bleeding, pain, or have noticed an enlarging lump, or changes in bowel movements, it is important to seek medical attention.
Taking action early is not overreacting; it is being responsible. In fact, the majority of individuals who develop cancers from HPV have no symptoms until the cancer is already well along in its development.
Living With High-Risk HPV: What That Actually Looks Like
The hardest part of testing positive for high-risk HPV is often the psychological aftermath. You leave the clinic or close your laptop, and suddenly the word “cancer” feels stitched to your body. But here’s what’s rarely said: most people with high-risk HPV live completely normal, healthy lives, and never develop cancer.
Living with HPV doesn’t mean you’re dirty or doomed. It means you’re human. It means you’ve encountered something 8 out of 10 sexually active adults will face in their lifetime. And now you have knowledge, something millions of others don’t, simply because they haven’t tested or haven’t been told.
HPV isn’t about who you slept with or how often. It’s about timing, immune response, and biology. You didn’t cause this. And you are not alone.
Reducing Long-Term Risk: What the Science Says
If you want to stack the deck against HPV-related cancer, prevention starts now, and it’s not complicated. Here's what studies consistently show:
Figure 2. Evidence-based prevention steps that reduce HPV persistence and cancer risk.
There’s no magic bullet, but each of these changes increases your chance of clearing the virus or keeping it from progressing.
The Stigma Still Sucks, But It’s Fading
Let’s not sugarcoat it, HPV stigma is real. Because it’s an STD, it often gets treated like a moral failing. That’s why people rarely disclose it, rarely talk about it, and rarely get the empathy they deserve after diagnosis.
But the culture is shifting. More and more people are speaking out about HPV, and medical organizations are pushing for inclusive, shame-free screening. You’ll even see public figures sharing their stories. The more we talk, the less isolated we feel, and the less power stigma has to harm us.
You don’t owe anyone your diagnosis. But you do deserve to move through this without shame.
Can HPV Come Back After It Clears?
Yes, and no. Once cleared, most people develop immunity to that strain. But HPV can behave unpredictably. Sometimes it becomes dormant and reappears later. Other times, reinfection occurs with a different partner or a different strain.
This doesn’t mean your body failed. It means HPV is a virus, and viruses do what they do. Retesting over time is normal. Staying in touch with your body and your screening schedule is what matters, not trying to control every microscopic detail.
Some providers offer immune panel testing or viral load screening to help understand HPV dynamics over time. But for most people, following standard care is enough.

People are also reading: Too Soon to Test? The Hepatitis B Window Period Explained
FAQs
1. Does high-risk HPV mean I’m going to get cancer?
Nope. A high-risk HPV result means your body encountered a strain that can lead to cancer, but it doesn’t mean you have it now, or ever will. Most people clear the virus on their own. The danger comes when it sticks around for years unnoticed, which is why screening matters. Think of this diagnosis less like a threat and more like a helpful heads-up.
2. Can you get rid of high-risk HPV?
There’s no magic pill for HPV, but your immune system is a beast. In fact, most people clear high-risk strains within one to two years without even realizing it. Staying healthy, sleeping, managing stress, not smoking, all that wellness advice your doctor gives you? It actually helps here.
3. Should I tell my partner I tested positive for high-risk HPV?
It depends on your situation, but yes, open communication is usually a good move. HPV is incredibly common, often passed without symptoms, and impossible to trace to a single person. You can frame it like, “Hey, I learned I have a common virus that a lot of people carry. It usually clears up on its own, but I want us to be informed together.”
4. Will having HPV affect my sex life?
Real talk: not unless you let it. HPV doesn’t mean you have to stop having sex, isolate, or panic. If anything, it’s a reason to learn more about your body and your boundaries. Barriers like condoms or dental dams can reduce risk. And communication? That’s the real aphrodisiac.
5. How long do I have to wait before retesting?
Usually 12 months, unless your provider says sooner. That wait can feel like forever, especially if you’re anxious, but retesting too soon doesn’t tell you much. Give your body time to clear the virus. And remember: persistence isn’t failure, it’s just information.
6. If I already have HPV, should I still get the vaccine?
Yes, it might still help. The HPV vaccine protects against multiple strains. Just because you’ve encountered one doesn’t mean you’ve had them all. It’s like locking other doors in your house, even if one’s already open, the others still matter.
7. Do guys need to worry about high-risk HPV too?
Absolutely. HPV doesn’t care about gender. Penile, anal, and throat cancers are real risks for people with penises, especially if they’re unvaccinated. Men who have sex with men and folks with HIV are at higher risk, but honestly, anyone who’s sexually active should be paying attention.
8. Can you test negative and still have HPV?
Unfortunately, yeah. No test is 100 percent accurate, and HPV can lay low. That’s why screening is important, not just a one-time thing. It’s like looking at pictures versus a video. You wouldn’t get the whole story from one picture, but you would from a video.
9. What’s the difference between HPV and genital warts?
They’re both caused by HPV, but different strains. Genital warts come from low-risk types like 6 and 11. High-risk HPV is the stuff linked to cancer. Warts are annoying but not dangerous; high-risk strains usually have no symptoms at all, and that’s what makes them tricky.
10. I tested positive but feel totally fine. Is that normal?
Totally. Most high-risk HPV infections come with zero symptoms. That’s why it’s called a “silent” virus. You’re not crazy for feeling weird about feeling normal. It just means the test did its job before the virus could do any damage. That’s a win.
You Deserve a Plan, Not Panic
Here’s the truth: being diagnosed with high-risk HPV is not the end of your story. It is, in fact, a turning point in your life, an opportunity to take control of your body, your health, and your life.
Whether you are dealing with a minor abnormality or coping with the stress of a new diagnosis, understand that you are not defective, you are not a threat, and you are not alone.
And if you're still unsure where to begin, don’t wait and wonder. This at-home combo test kit can check for the most common STDs quickly and discreetly, so you can focus on healing, not guessing.
How We Sourced This Article: We combined current guidance from leading medical organizations with peer-reviewed research and lived-experience reporting to make this guide practical, compassionate, and accurate. In total, around fifteen references informed the writing; below, we’ve highlighted some of the most relevant and reader-friendly sources.
Sources
1. WHO – HPV and Cervical Cancer Fact Sheet
2. Planned Parenthood – HPV Education & Prevention
3. About Genital HPV Infection – CDC
4. Basic Information About HPV and Cancer – CDC
5. HPV Infection & High-Risk Types – CDC Treatment Guidelines
About the Author
Dr. F. David, MD is a board-certified infectious disease specialist focused on STI prevention, diagnosis, and treatment. He blends clinical precision with a no-nonsense, sex-positive approach and is committed to expanding access for readers in both urban and off-grid settings.
Reviewed by: Jessica Lane, MPH | Last medically reviewed: January 2026
This article is for informational purposes and does not replace medical advice.