When Is the Right Time to Get Tested for HPV?
Quick Answer: Yes, certain STDs can lead to cancer, especially HPV, Hepatitis B, Hepatitis C, and HIV. These viruses can trigger or accelerate cancer development in the cervix, anus, liver, throat, and other areas. Regular screening, HPV vaccination, and early treatment are key ways to reduce this risk.
This Article Is for Anyone Who’s Ever Googled “STD and Cancer” at 2AM
If you’ve ever found yourself staring at your phone in the dark, scrolling through forums and asking if an STD could really lead to cancer, this article is for you. Whether you’re dealing with a recent diagnosis, worried about a past partner, or just trying to make informed decisions about your sexual health, you deserve clear, judgment-free answers. The fear is real. So is the confusion.
This guide is designed for anyone who’s:
- Trying to make sense of test results
- Worried about symptoms they can’t explain
- Living with HPV or HIV and wondering “what now?”
- Wondering if untreated infections from years ago could come back to haunt them
It doesn’t matter if you’re monogamous, poly, queer, straight, cis, trans, sexually active, or celibate. STDs don’t discriminate, and neither does cancer. What matters is knowledge, action, and self-compassion.
We’ll walk you through the STD–cancer connection with empathy, science, and clear language. You’ll also find testing resources, decision tools, and links to trusted guides like our STD Risk Checker Quiz to help you figure out your next steps based on your specific exposure history.
People are also reading: How (And Why) Gay Men Can Advocate for Better STD Testing
Let’s Get Specific: Which STDs Are Linked to Cancer?
Not all STDs are created equal when it comes to long-term risk. Some are bacterial and highly treatable with antibiotics. Others are viral and may stay in your system for life. Among the viral STDs, a few stand out for their strong, documented links to cancer, often in the cervix, throat, anus, penis, or liver. These include:
HPV is by far the most common cancer-linked STD, but it’s not the only one. The hepatitis viruses are often forgotten in the conversation, especially since many people don’t realize they can be transmitted sexually. HIV’s connection to cancer is more indirect, but very real, due to the way it dismantles immune protection over time.
Other STDs like chlamydia, gonorrhea, and syphilis are not directly linked to cancer but may play a role in increasing susceptibility. We’ll cover those subtler cases later in the article.
HPV: The Virus That Changes Cells Forever
Let’s start with HPV, because it’s the most well-known, and the most misunderstood. Human papillomavirus isn’t just one virus; it’s a family of more than 100 types, some of which are considered “high-risk.” These high-risk strains (especially types 16 and 18) are responsible for the vast majority of cervical cancer cases, as well as a large portion of anal and throat cancers.
The frustrating part? Most people who get HPV don’t know they have it. It doesn’t always cause warts, and it can live silently in the body for years. For some, it disappears on its own. But for others, it sticks around, slowly reshaping healthy cells into ones that grow uncontrollably. That’s cancer.
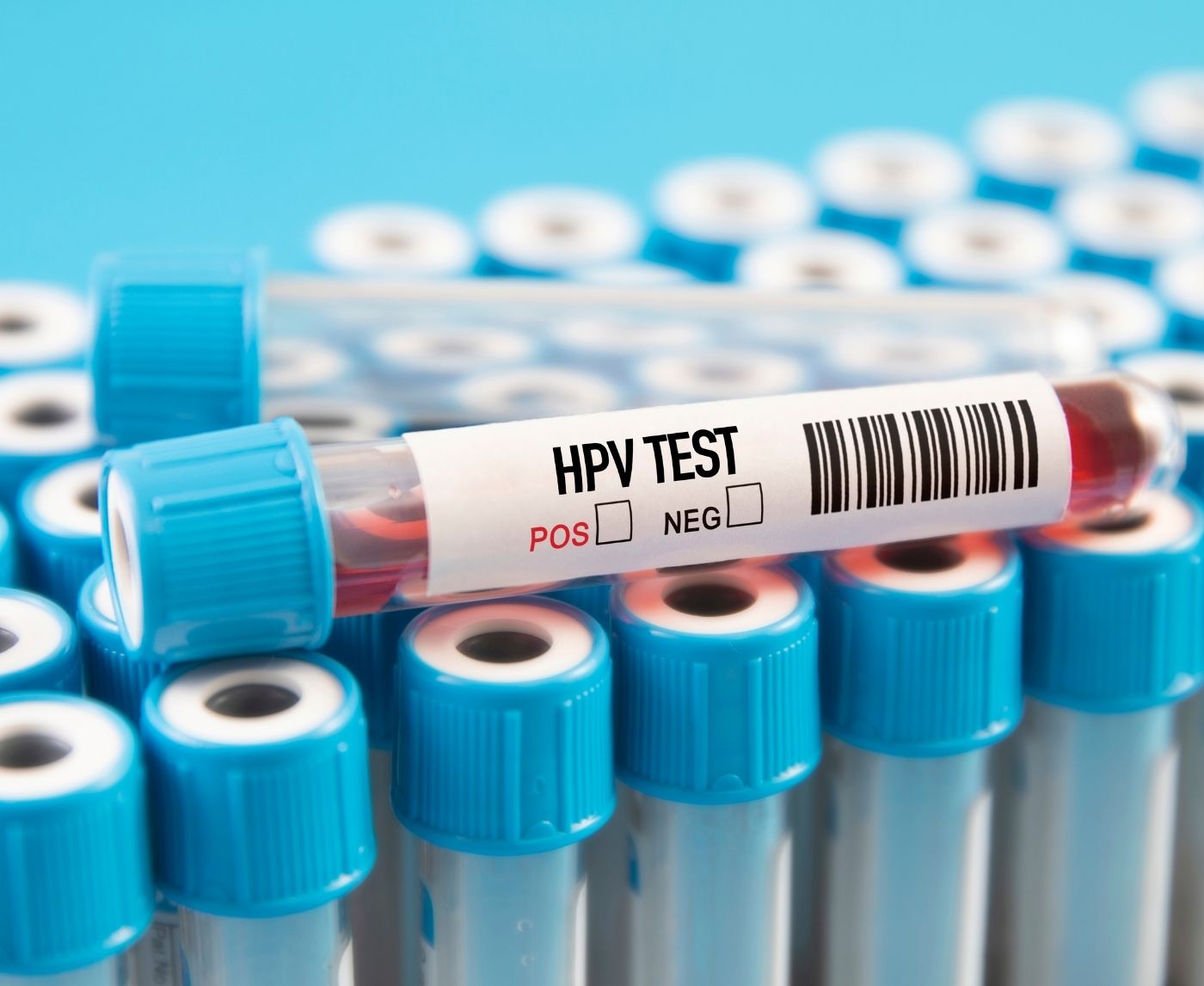
According to the Centers for Disease Control and Prevention, HPV causes about 36,000 cancers in men and women in the U.S. each year. Cervical cancer screening via Pap smear and HPV testing can catch cellular changes long before they become dangerous, which is why testing matters, even if you feel fine.
Want to know when to test for HPV or how long to wait after a new exposure? Our breakdown of STD window periods can help you figure out the best time to test for accurate results.
Hepatitis B and C: The Liver’s Slow Burn Toward Cancer
Elena was in her 40s when a routine blood panel revealed something unexpected, elevated liver enzymes. She didn’t drink, didn’t have a family history of liver issues, and had never used injectable drugs. After a follow-up screening, her doctor delivered the news: she had chronic hepatitis B, likely acquired years ago through unprotected sex. She felt fine. But her liver was quietly under siege.
Hepatitis B (HBV) and Hepatitis C (HCV) are viral infections that attack the liver and can be sexually transmitted, especially through condomless vaginal or anal sex, particularly when blood is involved. While not every case becomes chronic, the risk is real, and it’s the long-term, untreated cases that increase the chance of hepatocellular carcinoma, the most common type of liver cancer.
According to the CDC, chronic HBV affects over 800,000 people in the U.S., and many don’t know they have it. Hepatitis B is actually more infectious than HIV. That’s why there’s a vaccine, one that’s safe, effective, and underutilized. Hepatitis C doesn’t yet have a vaccine, but it does have curative antiviral treatment. Testing is crucial for both, especially for people who are sexually active, have had multiple partners, or were born between 1945 and 1965, a group with elevated risk.
Why does this matter in a conversation about cancer? Chronic inflammation in the liver, from the immune system constantly trying to fight the virus, causes damage that heals poorly. This repeated damage and repair can create scarring (cirrhosis), which increases the likelihood of cells turning cancerous. Liver cancer often has no early symptoms and is frequently diagnosed late, making prevention through testing and treatment especially vital.
HIV and Cancer: The Indirect Killer
When Andre got his HIV diagnosis, he wasn’t just overwhelmed by the virus itself, he was also shocked by what his doctor said next: “We’re going to monitor you for a few types of cancer.” It sounded like a death sentence. But as he later learned, it was just good medicine. Certain cancers are more common, and more aggressive, in people living with HIV.
HIV doesn't change cells into cancer like HPV does. Instead, it makes your whole body more vulnerable by slowly weakening your immune system. That means that viruses that your immune system would normally fight off, like Epstein-Barr, HHV-8, or high-risk HPV, are more likely to stick around and cause problems. People who are HIV-positive have a much higher risk of getting a number of specific cancers, such as:
People with HIV have such a high risk of getting cervical cancer that it is considered an AIDS-defining illness. Also, anal cancer rates are much higher, especially in men who have sex with men. But antiretroviral therapy (ART) has made a huge difference in the outcomes. When HIV is well-managed, the chances of getting cancer go down a lot. Regular checkups and screenings, such as Pap smears, anal Pap tests for people at high risk, and liver panels when there is coinfection, are the most important things.
Andre eventually got on ART, and his viral load became undetectable. With regular screenings, his care team stays ahead of potential problems. The fear hasn’t disappeared, but it’s no longer paralyzing. In his words: “Now I live. And I test. That’s how I stay in control.”
What About Chlamydia, Gonorrhea, and Syphilis?
This is where things get tricky. When people ask whether STDs cause cancer, they’re often thinking of the ones they’ve heard most about, the “big three” bacterial infections: chlamydia, gonorrhea, and syphilis. The answer is nuanced. These STDs do not directly cause cancer in the way viral infections like HPV or HBV do. But that doesn’t mean they’re harmless.
Let’s break it down. Chlamydia is a leading cause of pelvic inflammatory disease (PID) in women, which can cause long-term inflammation and scarring of reproductive organs. Some studies have shown a possible association between past chlamydia infection and increased risk of cervical cancer, not because chlamydia is oncogenic, but because inflammation may make HPV more likely to persist. Similarly, chronic gonorrhea may alter local immune response, making it harder for the body to clear high-risk HPV strains. However, these are associations, not proven causal relationships.
Syphilis, while extremely dangerous if left untreated, doesn’t cause cancer itself. But it does increase HIV transmission risk, and in advanced cases can compromise immune health in ways that make it harder for the body to deal with co-infections. In other words, these STDs don’t flip the cancer switch, but they may leave the door ajar.
That’s why treating all STDs quickly and thoroughly is a form of cancer prevention. It’s about breaking the chain, removing the conditions that allow precancerous processes to begin. When inflammation becomes chronic, when the immune system is worn down, and when viral co-infections go unchecked, cancer has a much easier time getting started.
Why Cancer Risk from STDs Is So Often Overlooked
When people think about STDs, they think about itching, discharge, maybe infertility. But cancer? That usually doesn’t make the list, and that’s part of the problem. We’ve framed STDs as short-term problems. Take a pill, wait a few days, and it’s over. But not all infections play by that rulebook. Some are silent. Some stick around. Some rewire your cells while you’re busy living your life.
STDs that raise cancer risk do it over years, not days. That’s why regular testing matters even when you feel fine. And that’s also why many people, especially those in monogamous relationships, stop screening. If nothing hurts and no one’s cheating, why test, right? But viral infections like HPV and hepatitis B can lie dormant for a decade or more. You may have been infected before your current relationship. You may have no idea it’s there.
Micah, a 35-year-old elementary school teacher, thought he was in the clear. He had no symptoms and hadn’t had a new partner in over five years. But after a routine physical flagged elevated liver enzymes, further tests revealed chronic hepatitis B. He was shocked, and even more stunned when his doctor mentioned liver cancer screening. “I didn’t even know hepatitis was an STD,” he said. “No one ever told me this was something I needed to test for.”
This gap in awareness is what allows cancer to grow in the shadows. Many STDs are preventable. Many related cancers are too, with the right combination of testing, vaccination, and treatment.

People are also reading: How to Know If That Eye Infection Might Actually Be an STD
Testing Isn’t Just About Symptoms, It’s About Timing
One of the most misunderstood aspects of STD-related cancer risk is when to test. People often test too early after exposure, or stop testing entirely after a negative result without understanding that some viruses take weeks or months to show up accurately.
That’s where resources like the STD Window Periods Guide become critical. It breaks down how long to wait after potential exposure to ensure your test results are as accurate as possible. For example:
These timelines matter. Testing too soon may give a false sense of safety. Waiting too long may delay care. If you’re unsure about your risk or when you last tested, our Risk Checker Quiz can help you figure out which infections you may need to screen for and when.
Remember, early detection isn’t just about peace of mind. It can literally be the difference between catching a precancerous lesion and a stage 3 diagnosis. You don’t have to be symptomatic to be proactive. Testing is care, not confession.
HPV Vaccines: Life-Saving, Misunderstood, and Underused
The HPV vaccine is one of the greatest public health wins of our time. Approved for people of all genders, it targets the high-risk HPV strains most likely to cause cancer. In countries with strong vaccine programs, cervical cancer rates have plummeted. But in the U.S., vaccine hesitancy and access gaps mean we’re still seeing thousands of preventable cancers each year.
Contrary to common myths, the vaccine doesn’t encourage promiscuity. It doesn’t affect fertility. And it’s not just for girls. Men benefit too, not only because HPV can cause throat, penile, and anal cancers, but also because reducing community transmission helps everyone.
Vaccination works best before you come into contact with the virus, which is why it is recommended that people start as young as 9 years old. But it might still protect you, even if you're older. Get in touch with your provider. You can always care about your future.
Another myth to bust: just because you get the vaccine doesn't mean you're immune to all strains. It protects against the most dangerous types, but you still need to get tested and follow screening guidelines. There isn't just one magic bullet for preventing cancer. There are layers of protection, testing, and monitoring.
Before You Panic, Here’s What to Do Next
If you’ve read this far, you’re likely carrying a mix of worry and relief. Worry, because yes, some STDs can absolutely increase your risk of cancer. But relief, because knowledge is power. And action is available. Testing, vaccines, and treatment work. They change lives. They save lives.
If you’ve never been tested or it’s been a long time, start there. Even if you're not showing symptoms. Even if you're in a monogamous relationship. Even if it feels scary. Especially if it feels scary. You don’t have to go to a clinic or explain yourself to a stranger. You can order a discreet kit directly from STD Test Kits and test from home, on your terms.
Most cancers linked to STDs are preventable. Many infections are treatable. The rest can be managed. What matters most is that you know your status and follow up when needed. That next step, clicking the order button, taking the test, scheduling the vaccine, that’s power. That’s protection. That’s love for your body.
FAQs
1. Wait, can you really get cancer from an STD?
Not from every STD, but yes, a few, especially viruses like HPV, hepatitis B, hepatitis C, and HIV, are linked to cancer. It’s not like one hookup = cancer; it’s more about long-term, untreated infections quietly affecting your cells over time. Think of it as a slow burn, not an explosion.
2. Which STD is most likely to lead to cancer?
Hands down, it’s HPV. Some strains are totally harmless, but the high-risk ones can cause cervical, anal, throat, and other cancers. Most people get HPV at some point, the key is whether your body clears it or it sticks around. That’s where Pap smears and HPV tests come in.
3. Can chlamydia or gonorrhea turn into cancer?
Not directly. They're bacterial infections, and cancer isn’t really their thing. But if left untreated for a long time, the inflammation they cause could make it easier for HPV to cause damage, like making your cervix more vulnerable. It’s more like setting the stage, not writing the script.
4. I tested positive for herpes. Should I be worried about cancer?
Nope. Herpes (HSV) causes painful outbreaks, not tumors. It can be a huge emotional stressor, but it’s not linked to cancer. That said, having herpes can slightly raise HIV transmission risk, and that’s where cancer concerns come in indirectly. Still, herpes itself isn’t on the cancer radar.
5. What about oral sex, can that lead to cancer too?
Yes, if you’re exposed to high-risk HPV strains during oral sex, it can increase your risk for throat cancer (specifically oropharyngeal cancer). You don’t need deep-throating or rough play for transmission, just skin-to-skin or mucosal contact. Protection helps, and the HPV vaccine is a game-changer here.
6. If I already got the HPV vaccine, am I totally safe?
You’re way safer, but not totally invincible. The vaccine protects against the most dangerous strains, but there are other types of HPV out there. It’s kind of like locking your doors, it doesn’t stop everything, but it drastically lowers your risk. Keep screening on schedule.
7. Should guys get the HPV vaccine too?
Yes, yes, and also yes. HPV doesn’t just cause cervical cancer. It’s behind a lot of throat, anal, and penile cancers too. The vaccine is approved for all genders, and the earlier you get it (ideally before any sexual contact), the better it works.
8. Can you test for these cancer-related STDs at home?
In most cases, yes. You can test at home for HIV, hepatitis B and C, and even HPV in some setups (like cervix swab kits). Just make sure you’re using a reputable provider. Pro tip: STD Test Kits has discreet options that ship fast and keep your business private.
9. How often should I test if I’m worried about cancer risk?
It depends on your sex life, your partners, and whether you’ve been vaccinated. Some folks test every 6 months, some yearly. If you’re living with HIV, have a cervix, or had an abnormal Pap, your doctor might suggest more frequent screenings. If you’re unsure, take the Risk Checker Quiz, it’ll give you a solid game plan.
10. If I’ve been with the same partner forever, do I still need to test?
Maybe. Infections like HPV and hepatitis can linger for years without symptoms. You could’ve been exposed in a past relationship or before you even knew your current partner. Testing isn’t about blame, it’s about taking care of your body, no matter your relationship status.
How We Sourced This Article: We combined current guidance from leading medical organizations with peer-reviewed research and lived-experience reporting to make this guide practical, compassionate, and accurate. In total, around fifteen references informed the writing; below, we’ve highlighted some of the most relevant and reader-friendly sources.
Sources
1. Chlamydia, Gonorrhea, and Cancer Risk Study (NIH/PMC)
2. National Cancer Institute – Infection and Cancer
3. Next Steps After Testing Positive for Gonorrhea or Chlamydia | CDC
5. Chlamydial Infections – STI Treatment Guidelines | CDC
About the Author
Dr. F. David, MD is a board-certified infectious disease doctor who focuses on preventing, diagnosing, and treating STIs. He combines clinical accuracy with a straightforward, sex-positive approach, and he wants to make it easier for readers to get to know him in both urban and rural areas.
Reviewed by: S. Greene, NP-C | Last medically reviewed: December 2025