Flu Symptoms After Sex? It Could Be Something Else
Quick Answer: HIV can worsen endometriosis flares by increasing immune system inflammation and disrupting hormone balance. Understanding the overlap helps you manage both with less pain and more clarity.
When Two Storms Collide: How HIV Amplifies Endometriosis
Endometriosis is already an inflammatory condition. The body treats endometrial-like tissue outside the uterus as an invader, sparking immune reactions and pain. HIV, even when well-managed, keeps the immune system in a state of low-grade activation. Combine them, and the inflammation multiplies.
Studies show that chronic immune activation in HIV alters cytokine levels, the same chemical messengers that regulate endo flares. When these are elevated, endometriotic lesions may grow or become more painful. One 2022 study noted that people with both conditions reported significantly worse menstrual symptoms than those with only one diagnosis.
Fatigue? That’s another shared symptom. And it’s not imagined. It stems from cytokine disruption, hormonal dysregulation, and the body constantly battling itself on two fronts. One reader put it best: “It’s like my uterus and my immune system are having a fight every month, and I’m the battlefield.”

People are also reading: What It Feels Like When Gonorrhea Travels to the Testicles
Case Study: “I Thought My Meds Were Causing the Pain”
Charmaine, 33, was diagnosed with HIV at 29 and had lived with endometriosis since her early 20s. For years, her pain had been managed with hormonal birth control and heating pads. But after starting antiretroviral therapy (ART), her symptoms shifted.
“I had these new waves of pelvic pain that didn’t match my cycle. I blamed the meds. But my OB-GYN said the HIV was probably making the endo worse.”
Her doctor explained how some HIV meds can indirectly affect estrogen levels. Others, like protease inhibitors, may influence inflammation pathways. It wasn’t that the meds were failing, it was that her body was juggling too much inflammation at once. Charmaine’s solution? A coordinated care plan between her infectious disease specialist and OB-GYN, with adjustments to both her ART and endo treatment. Her flares didn’t disappear, but they became more predictable, and more manageable.
If you're nodding along, you’re not alone. And you’re not imagining it.
What’s Really Causing the Flare? Immune vs Hormone Chaos
HIV impacts both sides of the equation: immunity and hormones. The immune system overreacts, and the hormonal cycle becomes less stable. Estrogen plays a huge role in endometriosis growth, and HIV can make estrogen levels unpredictable, especially if your meds or stress levels impact ovulation.
According to research published in the Journal of Women's Health, estrogen dominance and chronic inflammation are more pronounced in HIV-positive menstruators with endometriosis than in HIV-negative counterparts. This means your body is primed for pain, bloating, and longer or irregular periods.
Additionally, HIV-related inflammation may make your pelvic nerves more sensitive. So a flare that used to feel like a 5/10 pain scale now spikes to an 8. That’s not weakness, it’s biology. And it means you need a plan that addresses both systems, not just one.
When Testing Gets Confusing: Is It Endo or Something Else?
Pain during sex. Unusual discharge. Mid-cycle bleeding. These symptoms could be endometriosis, or signs of an STD. For people living with HIV, it’s especially important not to dismiss new symptoms as “just your endo acting up.” Coinfections are more likely when the immune system is compromised.
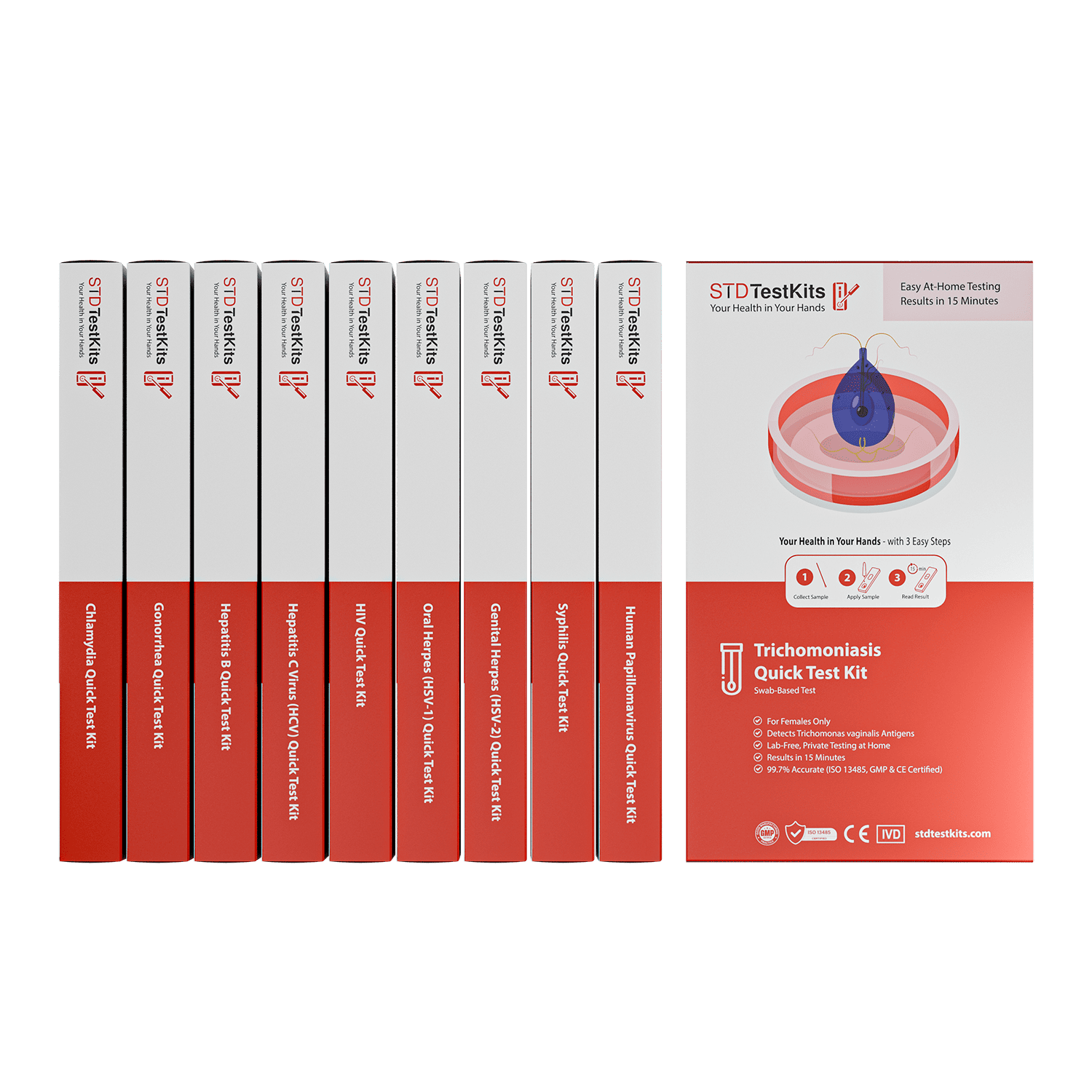
That’s why it’s smart to test regularly, even if you think you know what’s going on. You can order a discreet home test kit and get results in minutes. No judgment, no clinic wait. Just answers. If your symptoms are coming from something treatable like chlamydia or trichomoniasis, you can take action fast, before it worsens your endo or causes complications.
Testing doesn’t just rule things out, it gives you peace of mind. And when you’re already juggling HIV and endometriosis, that clarity is priceless.
Managing the Overlap: Treatment, Triggers, and What Works
There’s no one-size-fits-all approach to managing endometriosis, let alone when HIV is also in the picture. But one thing is consistent: inflammation is the enemy. Whether it’s your uterus shedding tissue or your immune system staying on high alert, the flares are usually driven by inflammatory overload. That means your care plan has to do more than control hormones or suppress viral load. It needs to address both at the same time.
Experts now recommend dual care teams, meaning your OB-GYN and infectious disease doctor should be talking to each other. Some ART medications can affect estrogen metabolism. Certain hormone therapies used for endo, like GnRH agonists, may impact your immune response. It’s a balancing act. And you deserve a team that helps you stay upright on that tightrope.
Tracking your cycle and flare patterns can also reveal if certain meds or timing align with worsened symptoms. Apps like Clue or paper journals can help. One HIV-positive reader shared:
“I realized every time I adjusted my ART dose, I’d have a flare. My doctor helped me space the timing better, and it changed everything.”
Hormonal Shifts, ART Meds, and Your Period
If you’ve noticed your periods are heavier, longer, or more painful since starting antiretroviral treatment, you’re not alone. Some people report cycle changes within months of ART initiation. While most of these are mild, in people with endometriosis, even small hormonal fluctuations can tip the balance into flare territory.
Certain ART drugs, especially older regimens, may interfere with estrogen processing in the liver. Others may reduce overall hormone levels. If you’re taking birth control to manage your endo, this could mean breakthrough bleeding or less effective flare control. Your provider might adjust your birth control type, timing, or combine it with pain management strategies.
For some, a progestin-only method (like a hormonal IUD or pill) works best because it limits endometrial buildup without triggering estrogen surges. For others, suppressing periods altogether may be the path of least pain. The key is to track, advocate, and tweak. This is where trauma-informed care matters, your pain is real, your lived experience is valid, and you deserve options that fit your body, not just your labs.
What Sex Looks Like When You Have Both
Painful sex (dyspareunia) is common with endometriosis, and HIV can complicate things further. Flare-ups might make vaginal penetration uncomfortable or even impossible during certain parts of your cycle. Add in concerns about viral load, STI risks, and communication with partners, and sex can start to feel like a minefield.
But here’s the truth: pleasure is still possible. You just need honest conversations, the right lube (water-based is usually best), and a partner, or partners, who listen. If you're undetectable, you can't transmit HIV. But it’s still smart to use condoms or dental dams, especially during flares when micro-tears from endo may increase vulnerability to other STIs.
If you’re navigating both conditions, you can check your status with a combo STD home test kit. Testing regularly keeps the guesswork out of intimacy, and lets you focus on connection, not fear.
Your sex life isn’t over. It just might look different. And that’s okay.

People are also reading: World Cup, Free Condoms, and What No One Talks About: STD Risks at Global Events
How to Know If It’s Time to Retest (Or Reassess)
When symptoms shift, whether it’s more bleeding, increased discharge, or sudden pelvic pain, it’s easy to brush it off as “just a bad endo day.” But if you’re HIV-positive, changes can also mean coinfections, med resistance, or even stress-related immune changes.
So how do you know when to test again?
Here’s the rule: if the pain feels different, if there’s a new symptom, or if it doesn’t track with your cycle, test. It’s that simple. Rapid test kits for trichomoniasis, gonorrhea, chlamydia, and syphilis are available for discreet, at-home use.
Testing isn’t a burden, it’s a boundary. It says, “I care about my health and my partners.” And it’s one of the most empowering things you can do, especially when juggling two chronic conditions.
Emotional Burnout Is Real, Here’s What Helps
You’re not weak for feeling overwhelmed. Chronic illness, especially two at once, is relentless. Many people with endo and HIV describe emotional burnout, medical fatigue, and periods of deep grief for the body they thought they had.
Whether it’s from pain, stigma, or just exhaustion, this toll matters. Mental health support is critical. That might look like a trauma-informed therapist, a support group, or even online communities like The Body or Reddit’s r/endometriosis and r/HIV. Wherever you find relief, take it.
One anonymous contributor shared:
“I used to feel ashamed of needing help. Now I schedule therapy like I schedule my bloodwork. It’s part of staying alive, not a luxury.”
You deserve that same support. You’re doing more than enough.
Planning for Flare Days: Your Mini Survival Blueprint
Some days, it hits out of nowhere: the ache, the brain fog, the stabbing pelvic pain that radiates into your thighs. Flare days are real, and if you’re living with both HIV and endometriosis, you need more than just ibuprofen and hope.
A personalized flare plan helps. Start with pain management: NSAIDs can be effective, but so can warmth, stretching, and switching ART timing if your doctor advises. Track which days in your cycle are worst and pre-plan rest or light duty around them. Stock up on what brings comfort: hot water bottles, rehydration packets, pelvic-friendly pillows, whatever works for you.
Nutrition and hydration matter too. Anti-inflammatory foods, like omega-3s, leafy greens, and berries, can help tone down the pain. And don’t underestimate hydration: both HIV and endometriosis can cause bloating, cramping, and nausea that water helps offset.
Finally, communicate with your circle. Whether that’s a partner, roommate, coworker, or chosen family, let someone know when you’re flaring. You don’t owe them details, but you do deserve support.
When Your Provider Doesn’t “Get It” (And What to Do)
Too many people living with chronic illness have faced it: a shrug, a dismissive glance, or the phrase, “It’s probably just stress.” For HIV-positive patients with pelvic pain, this is even more common. You deserve better.
If your doctor dismisses your endo symptoms because your labs look fine, consider this your permission to push back. Pain isn’t always visible on an ultrasound. Lesions aren’t always detectable unless laparoscopic surgery is done. And just because your viral load is undetectable doesn’t mean your inflammation is.
Look for providers who specialize in HIV and gynecologic care, or who are willing to consult others who do. Ask questions like: “How familiar are you with endometriosis in HIV-positive patients?” or “Are you open to a collaborative treatment plan?” If the answer is vague, or you leave feeling unseen, it’s okay to seek a second opinion. Your body is not up for debate.
And if you don’t know where to start, advocacy groups like the Endometriosis Foundation of America and the HIV Medicine Association offer directories and patient guides to help.
Testing, Tracking, and Tuning Into Your Body
When you're juggling both HIV and endometriosis, your body can feel like an unreliable narrator. But there’s power in the patterns, if you know where to look. Symptom tracking isn’t just for fertility apps or doctor visits. It’s a way of learning your body’s language.
Try noting when your fatigue spikes, when pain changes location, and how your meds correspond to symptoms. Use tags like “cycle day,” “med adjustment,” or “flare severity.” Over time, you may spot a correlation between a certain ART and your worst pain days, or notice that flares hit hardest after high-stress weeks.
Pair this with regular STD testing, not because you suspect something’s wrong, but because proactive health is preventative health. You can order a combo test kit here to screen for multiple infections in one go. Fast, private, no appointment required. Knowing your baseline makes it easier to spot what’s new, and act faster when something changes.
FAQs
1. Can HIV actually make endometriosis worse?
Yes, and it’s not just in your head. HIV keeps your immune system in a semi-alert state, which means more inflammation overall. For someone with endo, that’s like throwing gas on an already smoldering fire. You might feel like your cramps got meaner, your fatigue deeper, or your cycle more unpredictable. It’s not imaginary, it’s immunology.
2. Is it normal for my period to change after starting HIV treatment?
Totally. Some antiretroviral meds can shift your hormone balance or affect how your liver processes estrogen. That might mean longer cycles, heavier bleeding, or spotting when you didn’t expect it. If it feels different and disruptive, talk to your doctor, small med tweaks can make a big difference.
3. How can I tell if my pelvic pain is endometriosis or something else?
If you’ve had endo for a while, you probably know your body’s “usual pain playlist.” But if you notice new sensations, like sharper cramps, pain during peeing, discharge changes, or it just feels “off”, get tested. STDs like chlamydia or trich can absolutely mimic or worsen endo flares. Don’t guess. Test at home and know for sure.
4. What kind of birth control is best when you’ve got both HIV and endo?
Honestly, the one your body likes and doesn’t mess with your meds. Many HIV-positive folks do well with hormonal IUDs or progestin-only pills, they cut down bleeding without amping up estrogen, which can fuel endo flares. But every body is different. Your OB-GYN and HIV doc should be tag-teaming this with you.
5. Does being undetectable mean I can stop using condoms?
Being undetectable means you can’t transmit HIV, amazing news. But if you’ve got endo, which can cause micro-tears or bleeding, you might be more vulnerable to other STDs. So if you’re not in a monogamous, tested relationship, condoms still protect your peace (and your pelvis).
6. I feel exhausted all the time. Is it HIV or endo, or both?
Probably both. They’re a tag-team of fatigue. HIV can cause long-term immune fatigue even when your labs look great. Endo adds pain-related exhaustion, hormonal crashes, and sleep disruption. If you’re bone-tired, it’s not laziness, it’s your body doing too much, too often. Give it credit, and rest.
7. Can I still have a sex life with all this going on?
Hell yes. It might look different, maybe slower, maybe more communicative, maybe with more lube, but your pleasure doesn’t vanish just because you’ve got a couple diagnoses. Find what works for you, and don't settle for partners who act weird about it. Safe sex is hot, and consent is sexier than ever.
8. What do I do if my doctor brushes me off?
You fire them (gently, or not). If you’re being told “it’s probably stress” or “your labs look fine” while you’re doubled over in pain, that’s not care, it’s dismissal. Look for providers with HIV and endometriosis experience, or at least curiosity and compassion. You deserve better. Period.
9. How often should I test for STDs if I’m already HIV-positive?
Every 3 to 6 months is a solid rule of thumb, more often if you have new symptoms or partners. Coinfections can complicate HIV care and endo symptoms, so keep it simple: schedule it like you would a dentist appointment. Or better yet, keep a few combo test kits in your drawer for just-in-case clarity.
10. What’s one thing I can do today to feel more in control?
Track your flare. Seriously, jot down what hurts, when, how bad, and what you were doing before it started. Over time, you’ll notice patterns. That data is power. It tells you when to rest, when to test, and when to advocate harder. Your symptoms don’t have to be a mystery, they can be a map.
Before You Panic, Here’s What to Do Next
This isn’t in your head, and it’s not your fault. If you’re managing HIV and endometriosis, you’re living at the intersection of two systems that weren’t built to support your complexity. But your body still deserves care, and your story still deserves clarity.
You don’t have to wait for things to get worse. Whether you're questioning your pain, feeling overwhelmed by flares, or unsure if it’s something more, answers are a click away.
Order your discreet, FDA-approved combo STD home test kit today. Testing from home gives you fast results, peace of mind, and control when everything else feels uncertain.
How We Sourced This Article: We combined current guidance from leading medical organizations with peer-reviewed research and lived-experience reporting to make this guide practical, compassionate, and accurate. In total, around fifteen references informed the writing; below, we’ve highlighted six of the most relevant and reader-friendly sources. Every external link in this article was checked to ensure it leads to a reputable destination and opens in a new tab, so you can verify claims without losing your place.
Sources
1. HIV Medicine Association: Provider Directory
2. Endometriosis Overview (Office on Women’s Health, U.S. HHS)
3. Endometriosis - Symptoms and causes (Mayo Clinic)
4. Common Gynecologic Concerns for People Living with HIV (The Well Project)
5. HIV and Menstruation (ViiV Healthcare)
6. Menstrual symptoms and endometrial function in women with HIV (PubMed)
7. About HIV and AIDS (HIV.gov)
About the Author
Dr. F. David, MD is a board-certified infectious disease specialist focused on STI prevention, diagnosis, and treatment. He blends clinical precision with a no-nonsense, sex-positive approach and is committed to expanding access for readers in both urban and off-grid settings.
Reviewed by: Marla Jennings, MPH | Last medically reviewed: February 2026
This article is for informational purposes and does not replace medical advice.