Which STD Test Do I Need Based on My Symptoms?
Quick Answer: Symptoms of anal cancer that include bleeding, pain, or a lump can be similar to STD’s, hemorrhoids, or even infections. However, it’s always best to get tested as soon as possible when you are experiencing these symptoms and are at risk of having HPV.
Who This Is For: Anyone Wondering What That Bleeding Really Means
Maybe your partner noticed a trace of blood on the bedsheet. Maybe you’ve been having rectal pain during bowel movements or sex and told yourself it was just friction. Or maybe you’ve Googled “anal cancer from HPV” more than once and keep closing the tab before reading the results. This is for you.
This guide is especially relevant for:
- People assigned male at birth who have receptive anal sex, regardless of orientation
- Anyone with a history of HPV, HIV, or abnormal Pap smears
- People over 40 with persistent rectal symptoms
But even if none of those apply, your symptoms are valid. Your health deserves more than guesswork. This guide will walk you through symptoms, timelines, testing options, and what to do if something turns up.

People are also reading: When to Retest for Chlamydia: A Guide to Preventing Reinfection
Is Anal Cancer an STD?
Technically, no. Anal cancer itself is not a sexually transmitted disease. But in the overwhelming majority, or up to 91% of all cases, it is caused by certain strains of human papillomavirus, or HPV, which is one of the most common STDs in the world. In fact, more people are infected with HPV for anal cancer than for cervical cancer.
So, the virus that starts the process for anal cancer is spread through sexual contact. Most people will get rid of the virus within a short period of time, but in some, it will linger, causing cancerous cell changes.
Early Symptoms: When It’s More Than Just Hemorrhoids
Anal cancer is also diagnosed late in many patients simply because the symptoms are mistaken for more common, less serious conditions. These include hemorrhoids, fissures, or even STDs like gonorrhea, chlamydia, or herpes.
So, what does anal cancer feel like in real life? Here’s what patients have reported in the early stages:
Figure 1: Symptom comparison between anal cancer and STDs. Always consider duration, progression, and risk factors.
Case Study of a Missed Diagnosis
Jared, 38, had been dealing with occasional bleeding and discomfort for almost a year. His GP assumed hemorrhoids. Jared assumed it too, until his partner got tested and came back positive for high-risk HPV. Jared didn’t have warts. Didn’t feel sick. But a digital rectal exam and anoscopy found an early-stage tumor.
“I felt betrayed by my own body. But honestly? I was more scared of being judged than of dying. That’s what delayed me.”
Today, Jared’s in remission. But his story is a blunt reminder that shame kills. Early detection saves.
Is This Just an STD? Or Something Worse?
Most anal symptoms are NOT cancer. But they are worth checking. Common STDs like gonorrhea, chlamydia, and herpes can cause:
- Discharge
- Rectal pain
- Bleeding
- Itching
- Pain during or after sex
Some STDs also mimic each other, or cancer. HPV, especially, is confusing because it can cause visible warts, silent cell changes, or both. You may feel fine and still carry high-risk strains.
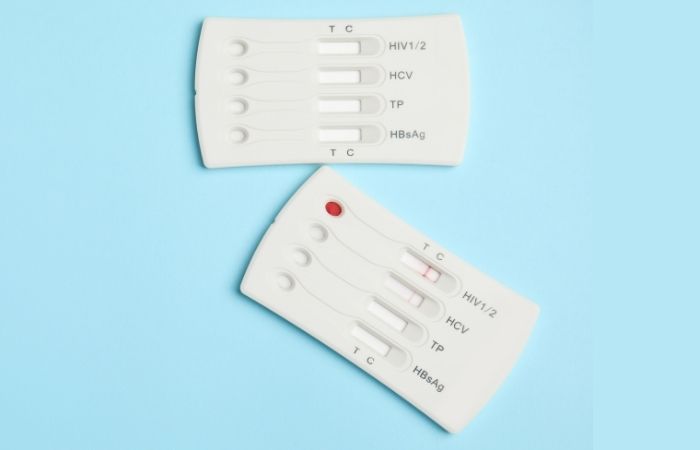
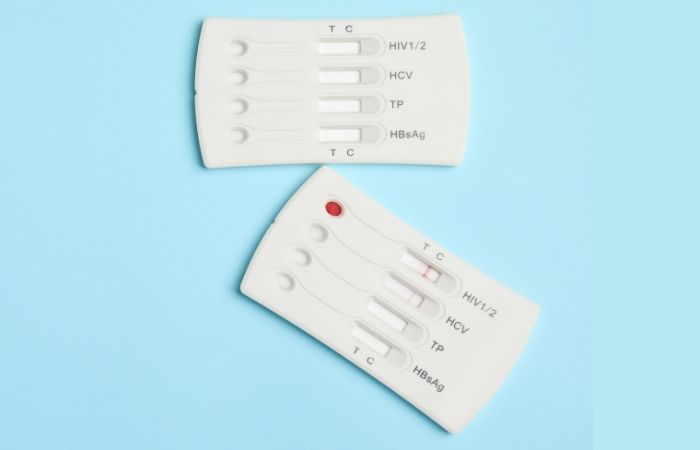
If you’re having symptoms or just anxious about a past encounter, there’s a way to get answers without walking into a clinic. This discreet combo STD test checks for multiple infections that could be behind your symptoms. It’s fast, private, and designed for people who don’t want to wait weeks for clarity.
Why HPV Is the Real Link Between STDs and Anal Cancer
Here’s the hard truth: HPV is the silent bridge between routine sexual activity and future cancer risk. It’s not just a “wart virus.” It’s the leading cause of anal, cervical, penile, throat, and vaginal cancers. Most sexually active people, up to 80%, will contract HPV at some point in their lives.
What makes HPV dangerous isn’t the initial infection, it’s the persistence. In most cases, the body clears the virus within one to two years. But when high-risk strains like HPV-16 or HPV-18 stick around, they can silently trigger cellular changes in the anal lining that evolve into anal intraepithelial neoplasia (AIN), a precursor to anal cancer.
Unlike cervical HPV, which is widely screened with Pap tests, there’s no universal anal HPV screening program. That’s why understanding risk, and self-advocating for testing, matters more than ever.
Who’s Most at Risk (And Why It’s Not Just About Orientation)
Anal cancer rates are rising, especially among certain populations. And while it disproportionately affects gay, bisexual, and other men who have sex with men (MSM), anyone can be at risk, regardless of gender identity or sexual orientation.
Figure 2: Key anal cancer risk groups and contributing factors. Data derived from CDC, NIH, and peer-reviewed studies.
Risk is not the same as destiny. But it should inform action, especially around screening, testing, and follow-up if symptoms appear.
How Do You Test for Anal HPV or Cancer?
HPV testing is not part of routine care for most individuals but can be ordered. If you are high-risk or are experiencing symptoms, it is a good idea to get tested. The following are available:
Anal Pap Smear: This is similar to a Pap smear performed on women. The test involves a swab of cells from the anal canal. The test checks for abnormal cells, not HPV. This is usually performed in a clinical setting, although some programs offer telemedicine services with a mail-out kit.
High-Risk HPV DNA Test: Some clinics and research studies offer a test that can determine if you are infected with high-risk HPV virus in the rectum. This test is usually performed with an anal Pap smear.
Digital Rectal Exam (DRE): This is a test where a physician feels for unusual masses inside the anus. This is a quick test that is usually covered by most insurances and is a necessary test for individuals over 40 years old who are experiencing symptoms.
At-Home STD Testing Kit: Although not a specific test for anal cancer, a test like the STD Rapid Combo Kit can test for diseases like gonorrhea, chlamydia, and herpes, which can cause symptoms similar to anal cancer or exacerbate HPV complications.
If you are stuck between a rock and a hard spot, trying to figure out where to begin, just remember that you can do something today. By ruling out STDs, you can narrow down where you should go next. And remember, peace of mind is part of treatment too!
Testing Windows: When to Swab, Scan, or Wait
Timing matters. Whether you’re testing for an STD, HPV, or suspicious rectal symptoms, the window period affects accuracy. Testing too early can lead to false reassurance, while waiting too long may delay treatment.
Here’s a simplified breakdown:
Figure 3: Recommended testing windows for STD-related and HPV-associated anal conditions.
Not sure where your exposure lands? You can use our Window Period Calculator to figure out the best time to test based on your situation.
What If the Test Is Negative, But You Still Have Symptoms?
This is where things get murky, and frustrating. Let’s say you’ve taken an at-home test. It came back negative for gonorrhea, chlamydia, and herpes. But the bleeding continues. Or the pain worsens. That’s your sign: it’s time to move past STD testing and ask your provider about anal cancer screening.
Here’s why: STDs can trigger short-term inflammation and symptoms, but if your body isn’t responding to treatment, or there’s a mass, persistent bleeding, or a “deep” kind of pain, there may be a cellular issue, not an infection. These aren’t symptoms to wait out.
Some people also test too early or don’t swab the right area. That’s why clinics may recommend repeat testing or send samples for anal cytology or biopsy if something feels off. If you’ve already tested negative for STDs, don’t stop there. A negative result doesn’t mean your experience isn’t real.
People are also reading: What a High-Risk HPV Diagnosis Means (And How to Protect Yourself)
Can Anal Cancer Be Prevented?
Not all things are in our control, but prevention still counts. These are the most effective tools we have:
HPV Vaccine: The HPV vaccine (Gardasil 9, for example) protects you against the high-risk types of HPV that are most likely to cause anal, cervical, and throat cancers. It’s FDA-approved for all individuals up to age 45 and is often covered by insurance.
Condoms and Barriers: They reduce, but don’t eliminate, the transmission of HPV. Since HPV can be transmitted through skin contact, barriers still reduce your risk of exposure and other infections.
Regular Screening (If You’re High-Risk): If you’re HIV-positive, MSM over 35, or have anal warts or cervical dysplasia, talk to your doctor about annual anal Pap tests and HPV DNA screening.
STD Testing and Treatment: Co-infections such as chlamydia and gonorrhea can increase the risk of HPV. Controlling other infections helps maintain healthy mucosa and prevents cancer-causing inflammation.
Let’s Talk About Fear, Stigma, and Waiting Too Long
Here’s the pattern we’ve seen, over and over: someone notices a symptom. They assume it’s from a toy, a rough night, or just hemorrhoids. They wait. Then they wait longer. Then the bleeding becomes daily. Then it’s harder to sit. But by the time they get checked, they’re dealing with Stage II or III cancer instead of a removable lesion.
The common thread? Shame. Fear of being judged for having anal sex. Embarrassment about disclosing symptoms. Anxiety about what a doctor will say.
But here’s the truth: Doctors see butts all day. They don’t care how yours got sore. What they care about is whether it’s cancer, an infection, or something treatable. And the earlier you get in, the easier it is to treat, no matter what it is.
If that’s not the provider vibe you’ve experienced, find a new one. You deserve care that respects your body and your autonomy.
In the meantime, home STD testing is a powerful first step. It’s not just about ruling things out, it’s about ruling yourself back in. Into your body. Into your power. Into the decision to act early, not late.
What If You’re Diagnosed With Anal Cancer?
First: breathe. Then know this, anal cancer is treatable, especially when caught early. Most cases are handled with radiation and chemotherapy. Some require surgery. The survival rate for early-stage cases is over 80%, and outcomes continue to improve as awareness and screening increase.
You may feel ashamed. Or furious. Or like your body betrayed you. That’s valid. But you’re not dirty. You’re not broken. You’re someone dealing with a serious but manageable diagnosis, and the system is finally catching up to help you through it.
Ask your provider about HPV testing for your partners. Discuss the timing of follow-up tests, recovery, and support. And know that you can, and should, still have a full, satisfying sex life after treatment. It may look different. But pleasure doesn’t disappear with diagnosis. Neither does dignity.
Whether your path starts with an itch or ends with a biopsy, you deserve truth without shame. And testing without barriers. Let’s make that happen.
FAQs
1. Can an STD actually turn into cancer?
Not exactly, but it is true. Some STDs, like HPV, do not cause cancer right away, but they prepare the way. Think of it this way: HPV is like an unwelcome guest who sneaks in unnoticed, sets up housekeeping in your cells, and if you do not throw it out, it rearranges the furniture. This is what can lead to anal cancer. STDs are not cancer, but cancer can be an STD.
2. I have bleeding down there, should I be worried?
If it’s a one-time thing after rough sex, a new toy, or straining on the toilet, maybe not. But if it’s happening more than once, especially if you’re not sure why, that’s your body asking you to check in. STDs like gonorrhea or chlamydia can cause bleeding. So can cancer. Bottom line? Recurrent bleeding = don’t ignore it.
3. How do I tell the difference between anal warts and something more serious?
Great question. HPV warts usually look like soft, skin-colored bumps or little cauliflower clusters. They might be itchy or annoying, but they’re not usually painful. A cancerous lesion, though? That’s more likely to feel firm, fixed, maybe ulcerated or bleeding. If it’s growing or just feels... wrong, get it checked. No shame in asking.
4. I tested negative for STDs, but I still have symptoms. Now what?
Then the next step is asking whether something deeper is going on, literally. Cancer, fissures, polyps, and inflammatory conditions can all mimic STDs. A negative test doesn’t mean you’re imagining it. It means it’s time to pivot your strategy and talk to a provider. You’re not crazy. You’re just not done yet.
5. Do only gay men get anal cancer?
Nope. That's a myth that needs to die already. While MSM, especially those who are HIV positive, are in a higher risk pool, anyone who has an anus and an HPV exposure history is in the potential risk pool. That includes cisgender women and trans folks as well as straight men.
6. Does HPV always come with visible warts?
Not even close. Most of the dangerous HPV strains, the ones that cause cancer, don’t cause warts at all. So don’t wait around for a bump to show up. You could feel totally fine and still be carrying high-risk strains. That’s why screening matters even when everything looks “normal.”
7. I’ve had HPV before, am I doomed to get cancer?
Not at all. Most people clear HPV without ever knowing they had it. Even if you’ve had abnormal cells in the past, with monitoring, treatment (if needed), and follow-up, the path doesn’t have to lead to cancer. This isn’t fate, it’s a risk factor. And risk factors can be managed.
8. Can I still hook up if I’m dealing with anal symptoms?
That depends on what the symptoms are. Mild irritation or healing hemorrhoids? Maybe. Ongoing bleeding or pain? Hit pause. Nobody’s judging you for having a sex life, but listen to your body. If sex feels scary or painful, it’s not your cue to push through, it’s your cue to get curious and get checked.
9. What if I’m embarrassed to talk to a doctor about this?
Totally fair. Anal symptoms carry a lot of stigma. But here’s the deal: your doctor has seen butts in every condition imaginable. They don’t care how you got there, they care what’s going on and how to help. If your current provider makes you feel judged, find another. You deserve respectful care.
10. Should I tell my partner I’m worried about cancer?
If you trust them and want their support, yes. But this is your body and your timeline. You’re allowed to gather facts first. If HPV’s involved or if you share sexual health history, looping them in can be empowering, not shameful. Start with: “Hey, I’ve noticed something weird and I’m getting it checked out. Just being proactive.”
You Deserve Answers, Not Assumptions
If you're still reading this, you care about your health, and that matters. Anal symptoms can be scary, but they’re also your body’s way of saying something’s not right. Whether it's an infection, inflammation, or early cancer, you have options. And you don’t have to wait to act.
Testing is not a confession. It’s a form of care. A way to reclaim clarity. A way to stop spinning and start healing.
Don’t wait and wonder, get the clarity you deserve. This at-home combo test kit checks for the most common STDs discreetly and quickly.
How We Sourced This Article: We combined current guidance from leading medical organizations with peer-reviewed research and lived-experience reporting to make this guide practical, compassionate, and accurate. In total, around fifteen references informed the writing; below, we’ve highlighted some of the most relevant and reader-friendly sources.
Sources
1. Anal Cancer — Symptoms and Causes (Mayo Clinic)
2. HPV and Cancer — Basic Information (CDC)
3. Anal Cancer Signs and Symptoms (American Cancer Society)
4. Anal Cancer: Symptoms, Causes & Treatment (Cleveland Clinic)
5. HPV-Associated Cancers Including Anal Cancer (CDC)
About the Author
Dr. F. David, MD, is a board-certified infectious disease specialist who focuses his practice on STI prevention, diagnosis, and treatment. He offers accuracy and a no-nonsense approach to sex that is positive and accessible to both urban and off-grid dwellers.
Reviewed by: Jasmine Keller, NP | Last medically reviewed: January 2026