Tested Too Soon for HIV? Here’s What That Negative Could Mean
Quick Answer: The best time to test for Hepatitis B is 6 weeks to 3 months after exposure. Early testing is possible, but results may not be reliable and retesting is often needed.
Who This Guide Is For (And Why It Matters)
This guide is for anyone sitting with that awful, electric anxiety after a possible exposure to Hepatitis B. You may be newly sexually active, recovering from an assault, questioning the reliability of a hookup, or just unsure if you’re overreacting. Maybe you’ve had a vaccine but aren’t sure if you’re protected. Maybe it was just a shared razor, and now you can’t sleep.
Danielle, 26, was two weeks into seeing someone new when she found out he used to inject drugs. She’d had oral and vaginal sex with him a few times, and now every itch, every twinge, made her wonder. She booked a same-day rapid test, hoping to calm down. It came back negative. But was that enough?
That’s what this guide is here to answer. We’ll cover what kind of test actually detects Hepatitis B, how long it takes to show up, what testing options exist (and what to avoid), and what to do if your first result is negative but your fear won’t quit.
People are also reading: My Balls Hurt, Do I Have an STD?
What Counts as a Real Hepatitis B Test?
There isn’t just one “Hepatitis B test.” There are a few different blood-based tests that look for different pieces of the virus, and the right one depends on when you were exposed and what you’re trying to find out.
The most common diagnostic tests include:
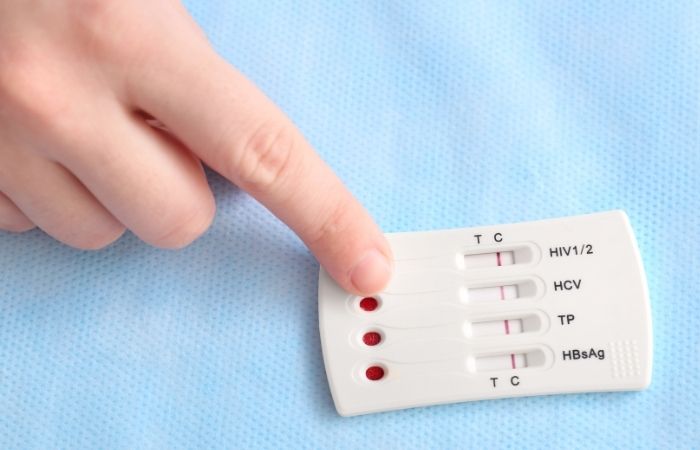
- HBsAg (Hepatitis B surface antigen): shows active infection; appears early and is used to detect acute cases.
- Anti-HBs (Hepatitis B surface antibody): shows immunity, either from past infection or vaccine.
- Anti-HBc (core antibody): can indicate recent or past infection, even when other markers are unclear.
In at-home kits or labs, these may be bundled together as a “Hepatitis B Panel.” If you’re testing on your own, make sure the kit checks for surface antigen (HBsAg), which is key for early detection.
To explore discreet, FDA-approved test options you can do from home, visit the STD Test Kits homepage or check out the Hepatitis B Rapid Test Kit.
Window Period vs Incubation Period: Why They’re Not the Same
This is where most confusion starts. You may feel fine. You may have symptoms. Either way, you can still be in the “window period”, a stretch of time after exposure where you’re infected, but the virus hasn’t built up enough to be detected by a test.
On average, Hepatitis B becomes detectable in blood within 30 to 60 days, but this can vary. And here’s the kicker: people can be infectious during this time, even if tests come back negative early on.
Figure 1. Window period vs incubation period: You can have Hepatitis B without symptoms, and testing before the window closes may give you false reassurance.
When Symptoms Don’t Help: Why You Can’t Trust How You Feel
Here’s one of the most frustrating truths about Hepatitis B: many people never have symptoms. Others don’t get sick until months after exposure. That means you can’t rely on how your body feels to decide whether to test, or when.
Alex, 32, felt completely fine after a vacation fling abroad. No fever, no rash, no yellowing of the eyes, nothing. It wasn’t until a friend mentioned hepatitis risks from unprotected sex that he considered testing. His first test, taken just 10 days after the last encounter, was negative. But 8 weeks later, follow-up bloodwork showed a positive result. His liver enzymes were already elevated.
This isn’t rare. The CDC reports that most acute Hepatitis B cases are asymptomatic. Even when symptoms do show up, they can mimic flu, fatigue, or food poisoning. The only way to know if you’re infected is to test, and to test at the right time.
When to Test: A Timeline That Actually Makes Sense
If you’re reading this in the panic spiral after a possible exposure, here’s how to navigate the decision-making process. Timing is everything, and testing too early may lead to a false negative that delays treatment, or spreads the infection unknowingly.
Figure 2. Hepatitis B detection timeline. This decision-support table helps determine when testing gives the most reliable result based on exposure date.
Not everyone fits these timelines exactly, and factors like immune response or co-infections (e.g., HIV) can affect results. That’s why medical professionals often recommend a two-step approach: one test early, one test after the window closes.
What Happens If You Test Too Early?
The biggest risk of early testing is false reassurance. You might get a negative result while still being in the window period, especially if you test within the first two weeks. This could lead you to skip follow-up testing, assume you're not infectious, or delay notifying partners, all while the virus continues to spread silently.
That’s exactly what happened to Lina, 40, who tested herself at home just 4 days after sharing needles with a partner. “I saw the one line and assumed I was okay,” she said. “I didn’t want to deal with a doctor. But I started feeling weak and nauseous a few weeks later.” Her follow-up test at 7 weeks confirmed she had acute Hepatitis B. If she had relied solely on the early result, she might have unknowingly put others at risk.
It’s not about blaming people, it’s about understanding biology and respecting the timing required for an accurate diagnosis.
If your head keeps spinning, peace of mind is one test away. You can explore discreet options like the Hepatitis B Test Kit or consult with a clinician for follow-up planning.
Retesting: Why One Test Isn’t Always Enough
Even if you’ve already tested once for Hepatitis B, that might not be the end of the story. Retesting can be essential, especially if your first test was taken during the early days after exposure. The goal isn’t to scare you. It’s to catch infections that take time to become detectable and make sure nothing slips through the cracks.
There are two common retesting scenarios:
- Early negative test (within 4 weeks): A follow-up test at 6 to 12 weeks can confirm the result.
- Symptoms after testing: If you test negative but develop nausea, fatigue, or jaundice later, retest, even if the first result was negative.
Marcus, 29, tested negative for Hepatitis B 10 days after a one-night stand. When nothing changed, he assumed he was safe. But a few weeks later, he developed dark urine and intense fatigue. A second test at week 8 came back positive, and his doctor caught it just in time to begin liver monitoring and supportive care.
If you’ve had ongoing exposure, like a sexual relationship with a positive partner, or repeated drug use with shared equipment, regular screening every few months is smart. Many clinics suggest a follow-up at 3 and 6 months in these cases.
Rapid Tests vs Mail-In vs Clinic: What’s Best for Hep B?
All Hepatitis B testing methods work by detecting the virus in your blood, but they vary in sensitivity, privacy, and turnaround time. Here’s how to think about your options:
Figure 3. Comparing Hepatitis B test methods. Choose based on timing, exposure risk, and what kind of peace of mind you need.
Some people start with a rapid test at home to get initial reassurance, then follow up with a lab-based or clinic test once the window period passes. There’s no wrong order, just remember to align timing with accuracy.
What If You’re Vaccinated? Do You Still Need to Test?
This one trips people up all the time. Yes, the Hepatitis B vaccine is highly effective, around 95%, but no vaccine is 100%. People with incomplete vaccine series, waning immunity, or immunosuppression may still be vulnerable.
If you're unsure about your protection, you can check your immunity status using a test for Anti-HBs. A result above 10 mIU/mL usually indicates immunity. Anything below that may mean you're not fully protected, even if you had shots years ago.
Tip: If you’re immunocompromised, pregnant, or work in healthcare, testing is often recommended after high-risk exposure even if you’ve been vaccinated. Talk to your provider about post-exposure prophylaxis (PEP) options like HBIG if exposure just happened.
Bottom line: don’t skip testing based on memory of shots alone. A simple blood test can clear it up.
What If Your Hepatitis B Test Comes Back Positive?
Take a breath. Seriously. Testing positive for Hepatitis B is heavy, but it’s not hopeless. Millions of people live full lives with HBV, and treatment, or close monitoring, can prevent serious complications. What matters most is catching it early and taking action.
If your result is positive, here’s what usually comes next:
- Confirmatory testing: Most labs or doctors will run a full Hep B panel to distinguish between acute, chronic, or past infection.
- Liver function tests: These check if the virus has begun affecting your liver.
- Partner notification: Hard but necessary. Some health departments can help notify partners anonymously.
- Care plan: Some people clear HBV on their own; others may need antiviral treatment or regular monitoring.
Drea, 24, got her results in a Walgreens parking lot. Her rapid test was positive. “I thought, ‘No one’s going to want me now.’” But within 48 hours, she had confirmation, a care team, and a plan. “It wasn’t the end. It was just a pivot.”
If you’re unsure what to do next, you can start by exploring at-home testing options for yourself or your partner. This rapid Hepatitis B test offers discreet, lab-grade results you can act on fast.

People are also reading: Tested Positive Without Having Sex? You’re Not Alone
FAQs
1. Can you test too early for Hepatitis B?
You definitely can, and a lot of people do, especially when panic sets in. It’s completely normal to want answers right away. But testing within the first couple of weeks can miss the virus entirely. That’s because Hepatitis B takes time to show up in your blood, think 30 to 60 days on average. Test too soon, and you might walk away with a false negative and a whole lot of false relief.
2. How soon after exposure does Hepatitis B usually show up in a test?
If you’re using a blood-based HBsAg test, most people will test positive between 4 and 8 weeks after exposure. That’s when the virus hits detectable levels. But if you’re immunocompromised or dealing with another infection, that timeline can stretch out. If you’re feeling unsure, it’s okay to test early, but plan to retest at the 6–12 week mark.
3. Is it possible to have Hepatitis B and feel totally fine?
Absolutely, and that’s what makes it so tricky. You could be going to work, hitting the gym, and living your life completely symptom-free while carrying the virus. That’s especially common in young adults. So don’t wait for symptoms like jaundice or nausea to show up. By the time they do, your liver’s already in distress.
4. Does a negative result mean I’m safe?
Not always. It depends on when you tested. A negative result within the first 2–3 weeks after exposure could mean you’re still in the “window period.” That’s why follow-up testing is so important, especially if you’re having ongoing sex with the same partner or if there was a high-risk exposure like shared needles.
5. I got the Hep B vaccine years ago. Do I still need to test?
Maybe. If you completed the full 3-dose series and your immune system is healthy, you’re probably protected. But immunity can fade over time, especially if it’s been a decade or more. If you’re unsure, there’s a quick blood test (Anti-HBs) that checks your protection level. If your titer is below 10 mIU/mL, you may want to boost or retest.
6. Can I use an at-home test for Hepatitis B?
Yes, and it’s becoming more common. Just make sure it checks for surface antigen (HBsAg), that’s what tells you if you have an active infection. At-home rapid tests are super helpful for quick reassurance, but if you're testing early, you’ll still want a lab follow-up to be sure. Think of it as your first step, not the final word.
7. Should I test again if my first result was negative?
If you tested before week 6? Yes. Especially if you’re still anxious, have new symptoms, or had unprotected sex again. One negative test isn’t a forever pass. The virus can be slow to show up, and it’s better to double-check than to play guessing games with your health.
8. Can Hepatitis B be cured?
Not exactly, but don’t panic. If it’s acute (caught early), your body can clear it naturally over a few months. If it becomes chronic, it’s manageable with regular care, monitoring, and in some cases, medication. Either way, knowing your status early gives you the power to protect your liver and avoid complications down the line.
9. Can Hepatitis B spread from kissing?
Very unlikely. The virus is not passed through saliva unless there’s bleeding involved (such as gums or sores in the mouth). The possible modes of transmission are: blood to blood contact, sex, razor blades, needles, and child birth. You’re in the clear unless kissing leads to more than kissing.
10. How do I tell someone they might’ve been exposed?
Start with honesty, not shame. You don’t need a script, you just need the facts. Try something like, “Hey, I tested for Hepatitis B recently and I think it’s important we both stay informed. I care about you and wanted to be upfront.” If that feels too hard, some health departments offer anonymous partner notification. Whatever route you take, it’s an act of care, not confession.
You Deserve Answers, Not Assumptions
Testing for Hepatitis B is more than just a medical task, it’s an emotional experience. Whether you’re testing after a risky night, a medical scare, or just for peace of mind, your timing matters. Too soon, and you might miss something. Too late, and you could delay care.
Don’t guess. Don’t Google in circles. Get the facts, get the test, and take control of your next step.
How We Sourced This Article: We combined current guidance from leading medical organizations with peer-reviewed research and lived-experience reporting to make this guide practical, compassionate, and accurate. In total, around fifteen references informed the writing; below, we’ve highlighted some of the most relevant and reader-friendly sources.
Sources
1. WHO – Hepatitis B Fact Sheet
2. Healthline – Understanding Hepatitis B
3. CDC: Testing for Hepatitis B — When and How It’s Done
4. Hepatitis B Foundation: Understanding Your Hepatitis B Test Results
5. Medscape: Hepatitis B — Serology, Diagnosis, and Timing of Tests
About the Author
Dr. F. David, MD is a board-certified infectious disease specialist focused on STI prevention, diagnosis, and treatment. He blends clinical precision with a no-nonsense, sex-positive approach and is committed to expanding access for readers in both urban and off-grid settings.
Reviewed by: J. Marquez, NP-C | Last medically reviewed: December 2025
This article is for informational purposes and does not replace medical advice.






